Hidden Non-Motor Symptoms of Parkinson’s Disease: Mood, Fatigue & Pain Explained


While the "visible" symptoms of Parkinson’s Disease (PD) like tremors and stiffness get the most attention, the "hidden" non-motor symptoms often take a greater toll on quality of life. These include depression, anxiety, fatigue, apathy, and pain. Because they are invisible, family members and even doctors may overlook them, leading to undertreatment and increased suffering for the patient.
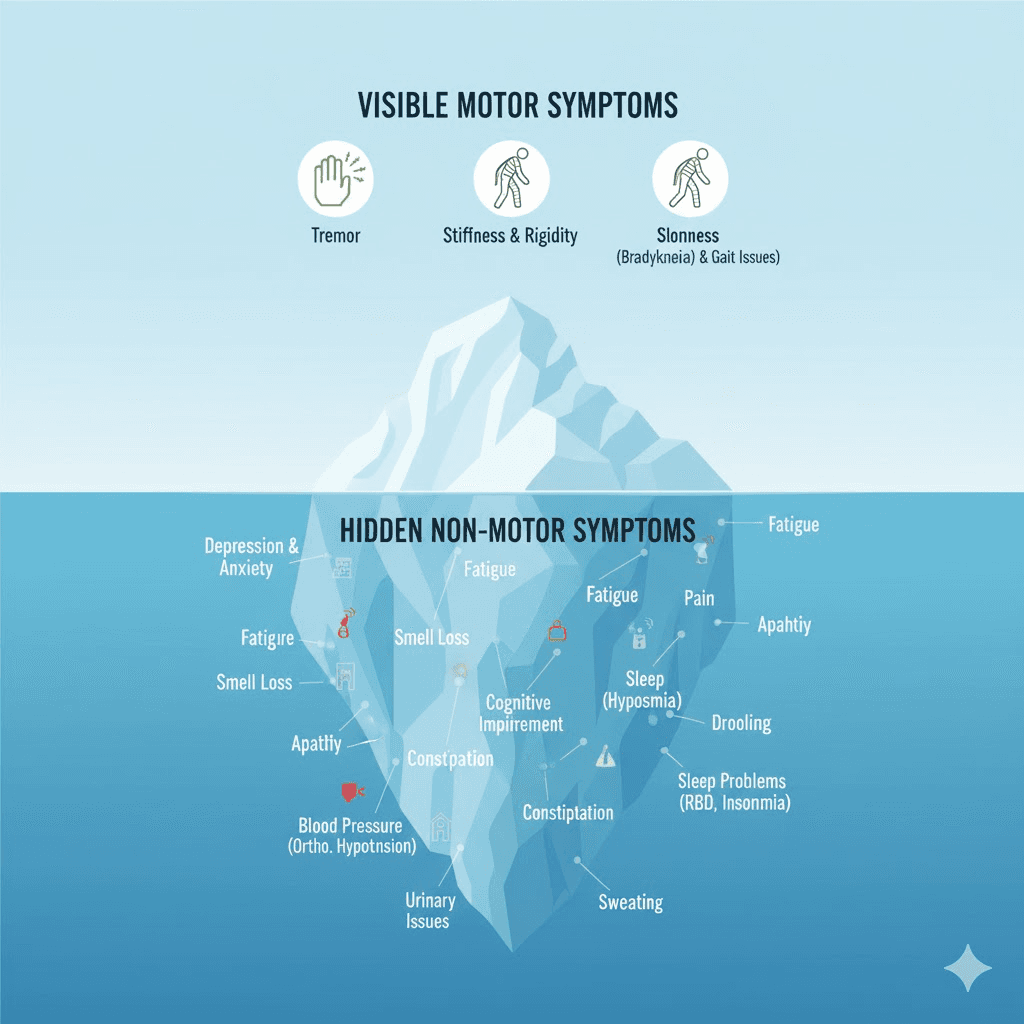
The Iceberg Analogy
Parkinson's Disease is often described as an iceberg. The tip of the iceberg—what everyone sees—is the tremor, the shuffle, and the masked face. But submerged beneath the surface is a massive chunk of symptoms that are invisible to the naked eye but felt deeply by the patient.
The Invisible Burden
1. Mood Disorders (Depression and Anxiety)
Biological, not just reactive: Depression in PD isn't just sadness about the diagnosis; it's caused by the lack of dopamine and serotonin, the brain's "feel-good" chemicals.
Anxiety: Up to 40% of patients experience severe anxiety, often manifesting as panic attacks during "OFF" periods (when medication wears off).
2. Fatigue
Bone-weary tiredness: This isn't just being sleepy. It's a profound exhaustion that doesn't go away with rest. It makes every task feel like climbing a mountain.
3. Apathy
The "Don't Care" Syndrome: Patients may lose interest in hobbies they used to love. This is often mistaken for laziness or depression, but it's a distinct lack of motivation caused by frontal lobe dysfunction.
4. Pain
Unexplained aches: About 80% of PD patients report pain. It can be musculoskeletal (from rigidity), neuropathic (burning/tingling), or dystonic (muscle twisting).
5. Autonomic Dysfunction
Sweating: Excessive sweating (hyperhidrosis), especially at night or during "OFF" periods.
Temperature Dysregulation: Feeling freezing cold or burning hot regardless of the weather.
Why Are They "Hidden"?
Communication barriers: Patients with a soft voice or masked face may struggle to express their feelings.
Focus on motor skills: Doctors appointments are often short and focus on "How is your walking?" rather than "How is your mood?"
Embarrassment: Issues like incontinence or sexual dysfunction are hard to talk about.
Bringing Them to Light
1. The Non-Motor Symptoms Questionnaire (NMSQuest)
This is a checklist patients can fill out before seeing their doctor. It covers everything from dribbling saliva to vivid dreams. Using this tool ensures nothing is missed.
2. Integrated Care
Treating PD requires a team, not just a neurologist.
Psychiatrist/Psychologist: For mood and anxiety.
Pain Specialist: For chronic pain management.
Social Worker: For family support and resources.
3. Education for Caregivers
Family members need to know that when their loved one sits in a chair for hours, it might be apathy, not stubbornness. When they snap in anger, it might be anxiety, not meanness.
Key Takeaways
Speak up: Your doctor can't treat what they don't know about.
Treatable: Most non-motor symptoms respond well to medication or therapy.
Quality of Life: Treating depression or pain often improves life satisfaction more than fixing the tremor.
Holistic view: You are a whole person, not just a collection of moving parts.
FAQ
Q: Is pain common in early Parkinson's?
A: Yes, unexplained shoulder or hip pain is a common early symptom, often occurring before the diagnosis is even made.
Q: Can fatigue be treated?
A: It's difficult, but stimulants (like modafinil) or exercise programs can help. Conserving energy for important tasks is also key.
Q: Why do I sweat so much?
A: It's a sign of autonomic instability. It often happens when your medication is wearing off.
While the "visible" symptoms of Parkinson’s Disease (PD) like tremors and stiffness get the most attention, the "hidden" non-motor symptoms often take a greater toll on quality of life. These include depression, anxiety, fatigue, apathy, and pain. Because they are invisible, family members and even doctors may overlook them, leading to undertreatment and increased suffering for the patient.
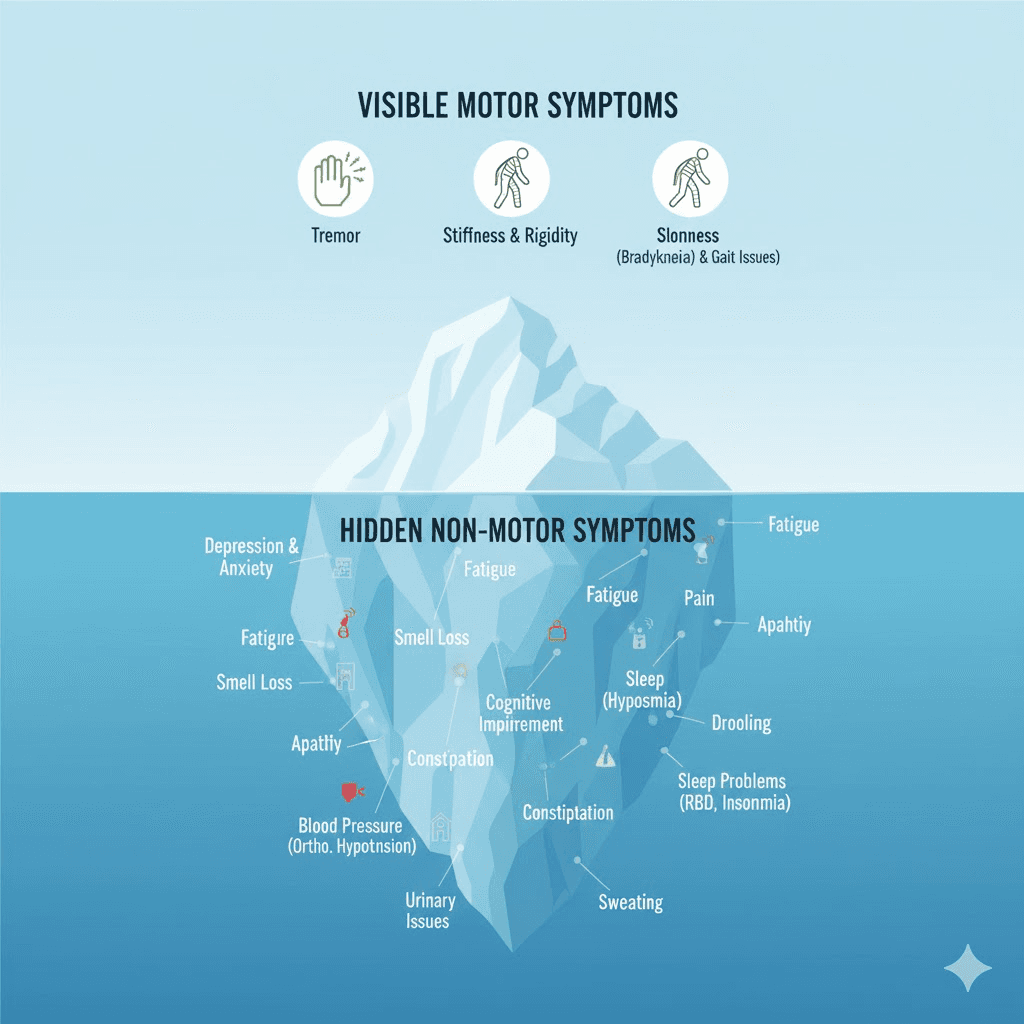
The Iceberg Analogy
Parkinson's Disease is often described as an iceberg. The tip of the iceberg—what everyone sees—is the tremor, the shuffle, and the masked face. But submerged beneath the surface is a massive chunk of symptoms that are invisible to the naked eye but felt deeply by the patient.
The Invisible Burden
1. Mood Disorders (Depression and Anxiety)
Biological, not just reactive: Depression in PD isn't just sadness about the diagnosis; it's caused by the lack of dopamine and serotonin, the brain's "feel-good" chemicals.
Anxiety: Up to 40% of patients experience severe anxiety, often manifesting as panic attacks during "OFF" periods (when medication wears off).
2. Fatigue
Bone-weary tiredness: This isn't just being sleepy. It's a profound exhaustion that doesn't go away with rest. It makes every task feel like climbing a mountain.
3. Apathy
The "Don't Care" Syndrome: Patients may lose interest in hobbies they used to love. This is often mistaken for laziness or depression, but it's a distinct lack of motivation caused by frontal lobe dysfunction.
4. Pain
Unexplained aches: About 80% of PD patients report pain. It can be musculoskeletal (from rigidity), neuropathic (burning/tingling), or dystonic (muscle twisting).
5. Autonomic Dysfunction
Sweating: Excessive sweating (hyperhidrosis), especially at night or during "OFF" periods.
Temperature Dysregulation: Feeling freezing cold or burning hot regardless of the weather.
Why Are They "Hidden"?
Communication barriers: Patients with a soft voice or masked face may struggle to express their feelings.
Focus on motor skills: Doctors appointments are often short and focus on "How is your walking?" rather than "How is your mood?"
Embarrassment: Issues like incontinence or sexual dysfunction are hard to talk about.
Bringing Them to Light
1. The Non-Motor Symptoms Questionnaire (NMSQuest)
This is a checklist patients can fill out before seeing their doctor. It covers everything from dribbling saliva to vivid dreams. Using this tool ensures nothing is missed.
2. Integrated Care
Treating PD requires a team, not just a neurologist.
Psychiatrist/Psychologist: For mood and anxiety.
Pain Specialist: For chronic pain management.
Social Worker: For family support and resources.
3. Education for Caregivers
Family members need to know that when their loved one sits in a chair for hours, it might be apathy, not stubbornness. When they snap in anger, it might be anxiety, not meanness.
Key Takeaways
Speak up: Your doctor can't treat what they don't know about.
Treatable: Most non-motor symptoms respond well to medication or therapy.
Quality of Life: Treating depression or pain often improves life satisfaction more than fixing the tremor.
Holistic view: You are a whole person, not just a collection of moving parts.
FAQ
Q: Is pain common in early Parkinson's?
A: Yes, unexplained shoulder or hip pain is a common early symptom, often occurring before the diagnosis is even made.
Q: Can fatigue be treated?
A: It's difficult, but stimulants (like modafinil) or exercise programs can help. Conserving energy for important tasks is also key.
Q: Why do I sweat so much?
A: It's a sign of autonomic instability. It often happens when your medication is wearing off.
While the "visible" symptoms of Parkinson’s Disease (PD) like tremors and stiffness get the most attention, the "hidden" non-motor symptoms often take a greater toll on quality of life. These include depression, anxiety, fatigue, apathy, and pain. Because they are invisible, family members and even doctors may overlook them, leading to undertreatment and increased suffering for the patient.
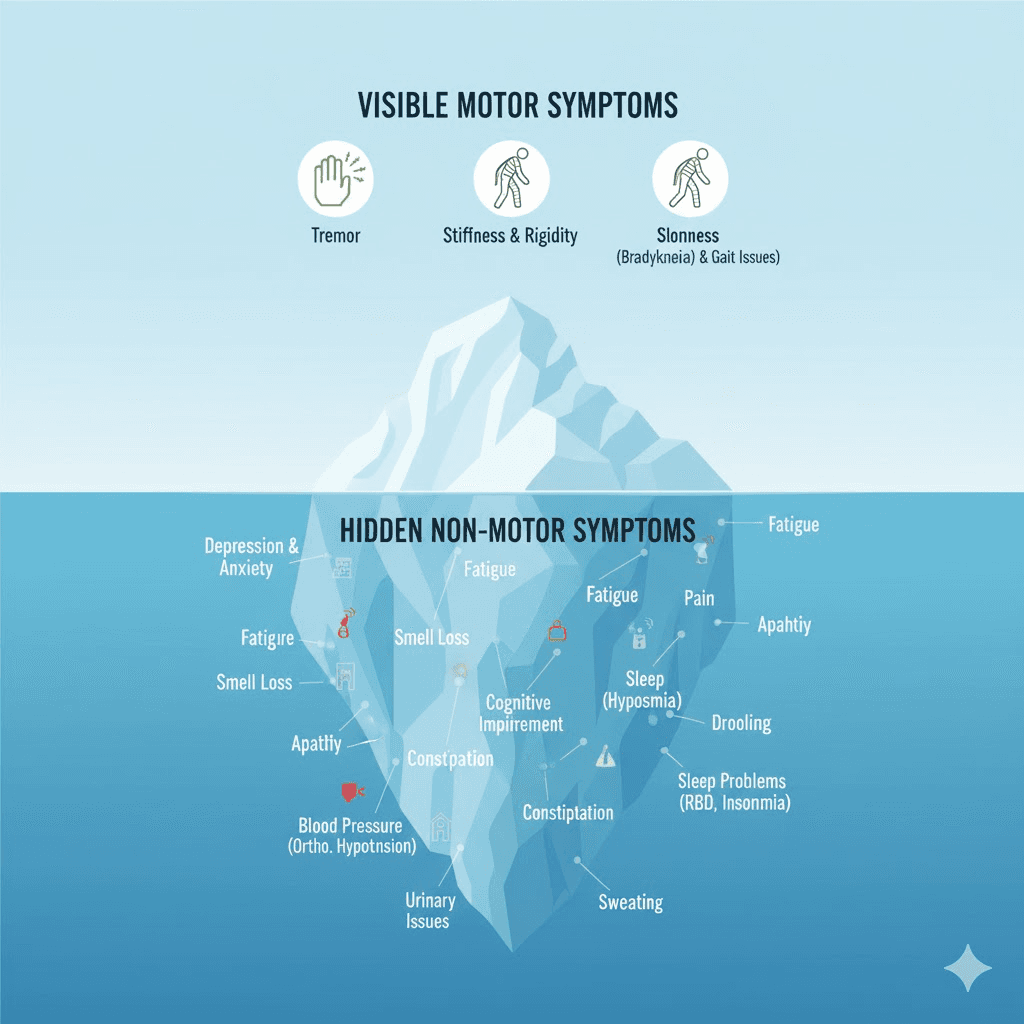
The Iceberg Analogy
Parkinson's Disease is often described as an iceberg. The tip of the iceberg—what everyone sees—is the tremor, the shuffle, and the masked face. But submerged beneath the surface is a massive chunk of symptoms that are invisible to the naked eye but felt deeply by the patient.
The Invisible Burden
1. Mood Disorders (Depression and Anxiety)
Biological, not just reactive: Depression in PD isn't just sadness about the diagnosis; it's caused by the lack of dopamine and serotonin, the brain's "feel-good" chemicals.
Anxiety: Up to 40% of patients experience severe anxiety, often manifesting as panic attacks during "OFF" periods (when medication wears off).
2. Fatigue
Bone-weary tiredness: This isn't just being sleepy. It's a profound exhaustion that doesn't go away with rest. It makes every task feel like climbing a mountain.
3. Apathy
The "Don't Care" Syndrome: Patients may lose interest in hobbies they used to love. This is often mistaken for laziness or depression, but it's a distinct lack of motivation caused by frontal lobe dysfunction.
4. Pain
Unexplained aches: About 80% of PD patients report pain. It can be musculoskeletal (from rigidity), neuropathic (burning/tingling), or dystonic (muscle twisting).
5. Autonomic Dysfunction
Sweating: Excessive sweating (hyperhidrosis), especially at night or during "OFF" periods.
Temperature Dysregulation: Feeling freezing cold or burning hot regardless of the weather.
Why Are They "Hidden"?
Communication barriers: Patients with a soft voice or masked face may struggle to express their feelings.
Focus on motor skills: Doctors appointments are often short and focus on "How is your walking?" rather than "How is your mood?"
Embarrassment: Issues like incontinence or sexual dysfunction are hard to talk about.
Bringing Them to Light
1. The Non-Motor Symptoms Questionnaire (NMSQuest)
This is a checklist patients can fill out before seeing their doctor. It covers everything from dribbling saliva to vivid dreams. Using this tool ensures nothing is missed.
2. Integrated Care
Treating PD requires a team, not just a neurologist.
Psychiatrist/Psychologist: For mood and anxiety.
Pain Specialist: For chronic pain management.
Social Worker: For family support and resources.
3. Education for Caregivers
Family members need to know that when their loved one sits in a chair for hours, it might be apathy, not stubbornness. When they snap in anger, it might be anxiety, not meanness.
Key Takeaways
Speak up: Your doctor can't treat what they don't know about.
Treatable: Most non-motor symptoms respond well to medication or therapy.
Quality of Life: Treating depression or pain often improves life satisfaction more than fixing the tremor.
Holistic view: You are a whole person, not just a collection of moving parts.
FAQ
Q: Is pain common in early Parkinson's?
A: Yes, unexplained shoulder or hip pain is a common early symptom, often occurring before the diagnosis is even made.
Q: Can fatigue be treated?
A: It's difficult, but stimulants (like modafinil) or exercise programs can help. Conserving energy for important tasks is also key.
Q: Why do I sweat so much?
A: It's a sign of autonomic instability. It often happens when your medication is wearing off.

