Diagnosing Parkinson’s Disease


Diagnosing Parkinson’s Disease (PD) is a clinical process, meaning there is no single lab test or scan that can confirm it 100%. Neurologists rely on a detailed medical history and a physical examination to look for the cardinal signs: tremor, slowness of movement (bradykinesia), and muscle stiffness (rigidity). Specialized tests like the Levodopa Challenge Test or DaTscan (Dopamine transporter scan) may be used to support the diagnosis and rule out other conditions.
The Puzzle of Diagnosis
Parkinson's Disease cannot be identified by a simple blood draw. It is a "diagnosis of exclusion," meaning doctors must rule out other conditions that mimic PD symptoms before confirming the diagnosis. This process can sometimes take time, as symptoms often develop slowly.
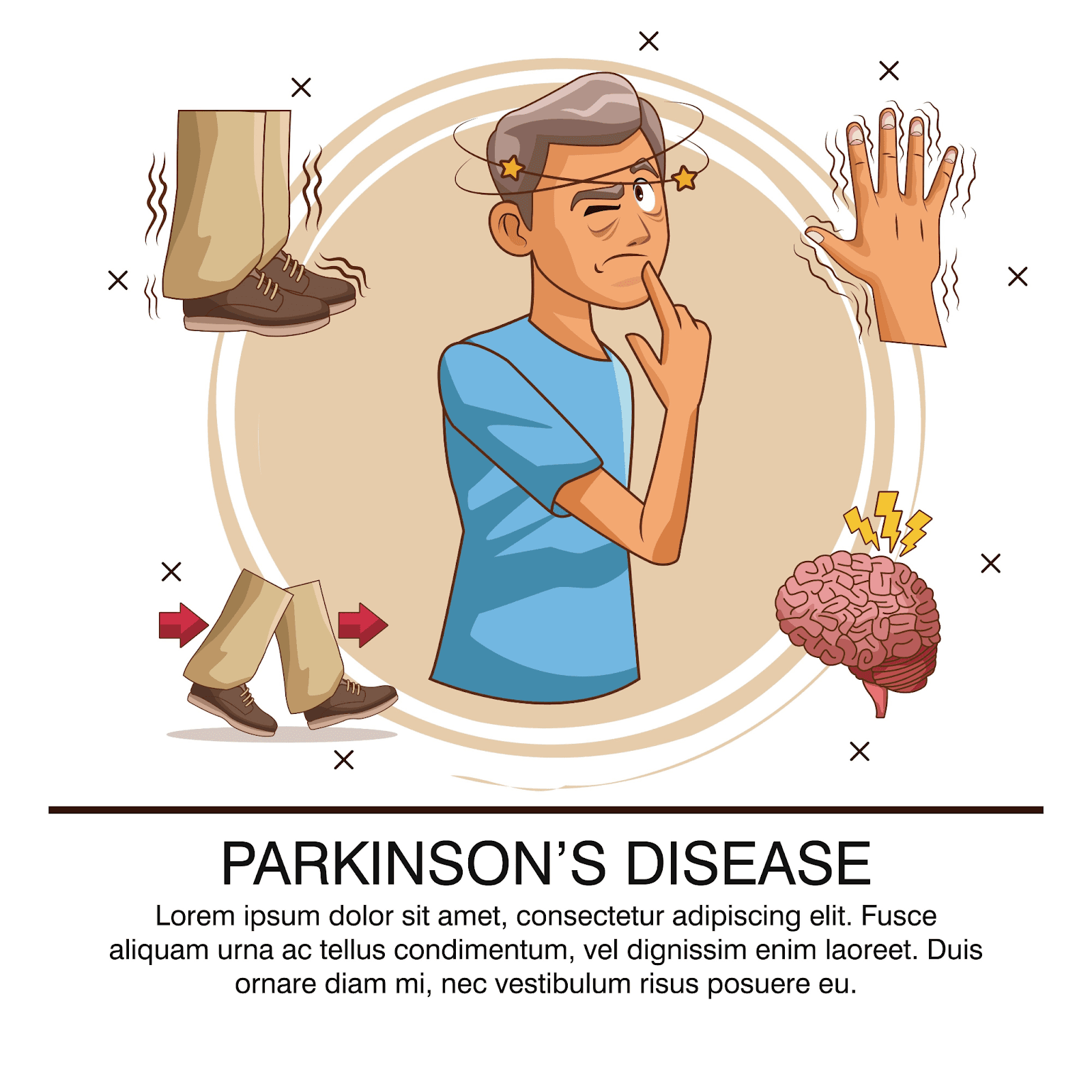
The Cardinal Symptoms (TRAP)
Neurologists look for the presence of at least two of the four primary symptoms for a diagnosis.
T - Tremor: Usually a "resting tremor" that happens when the limb is relaxed, often described as "pill-rolling" with the thumb and forefinger.
R - Rigidity: Stiffness in the limbs or trunk. The doctor may feel "cogwheel rigidity" (a ratchet-like stop-and-go movement) when moving the patient's arm.
A - Akinesia / Bradykinesia: Slowness of movement. This is often tested by asking the patient to tap their fingers quickly or stomp their foot.
P - Postural Instability: Impaired balance and coordination, often leading to falls. (This usually appears in later stages).
Here is an infographic summarizing the key symptoms of Parkinson's Disease:
The Diagnostic Process
1. Medical History
The doctor will ask about:
When symptoms started.
Family history of neurological disorders.
Exposure to toxins (pesticides, heavy metals).
Current medications (some drugs can cause Parkinson-like symptoms).
2. Physical and Neurological Exam
Observation: Checking for reduced facial expression (masked face), soft voice, or lack of arm swing while walking.
Motor Tests: Assessing muscle tone, agility, and balance.
3. Response to Medication
A significant improvement in symptoms after taking Levodopa (a dopamine replacement drug) is a strong indicator of Parkinson's Disease. This is often formalized as a "Levodopa Challenge Test."
4. Imaging Tests
MRI / CT Scan: These are mainly used to rule out other causes like strokes, tumors, or hydrocephalus. Normal PD brains often look normal on these scans.
DaTscan: A specialized imaging test that visualizes the dopamine transporter system in the brain. It can distinguish between Essential Tremor and Parkinsonian syndromes but cannot differentiate between PD and atypical parkinsonism (like MSA or PSP).
Early Warning Signs
Diagnosis often happens after motor symptoms appear, but non-motor signs can precede them by years:
Loss of smell (Anosmia).
REM Sleep Behavior Disorder: Acting out dreams, kicking, or punching while asleep.
Constipation.
Small handwriting (Micrographia).
Key Takeaways
No single test: Diagnosis is a combination of history, exam, and observation.
Expertise matters: A Movement Disorder Specialist (a type of neurologist) is best equipped to make an accurate diagnosis.
It takes time: Sometimes a diagnosis is "Probable Parkinson's" until the disease progresses or responds to medication.
Rule out others: It's crucial to ensure symptoms aren't caused by medication side effects or other neurological conditions.
FAQ
Q: Can stress cause Parkinson's?
A: Stress doesn't cause Parkinson's, but it can make symptoms like tremors temporarily worse.
Q: Is Parkinson's genetic?
A: In most cases (about 85-90%), it is not directly inherited. However, having a close relative with PD slightly increases the risk.
Q: What is the difference between Essential Tremor and Parkinson's?
A: Essential Tremor usually happens during action (like holding a cup), while Parkinson's tremor happens when the hand is at rest.
Diagnosing Parkinson’s Disease (PD) is a clinical process, meaning there is no single lab test or scan that can confirm it 100%. Neurologists rely on a detailed medical history and a physical examination to look for the cardinal signs: tremor, slowness of movement (bradykinesia), and muscle stiffness (rigidity). Specialized tests like the Levodopa Challenge Test or DaTscan (Dopamine transporter scan) may be used to support the diagnosis and rule out other conditions.
The Puzzle of Diagnosis
Parkinson's Disease cannot be identified by a simple blood draw. It is a "diagnosis of exclusion," meaning doctors must rule out other conditions that mimic PD symptoms before confirming the diagnosis. This process can sometimes take time, as symptoms often develop slowly.
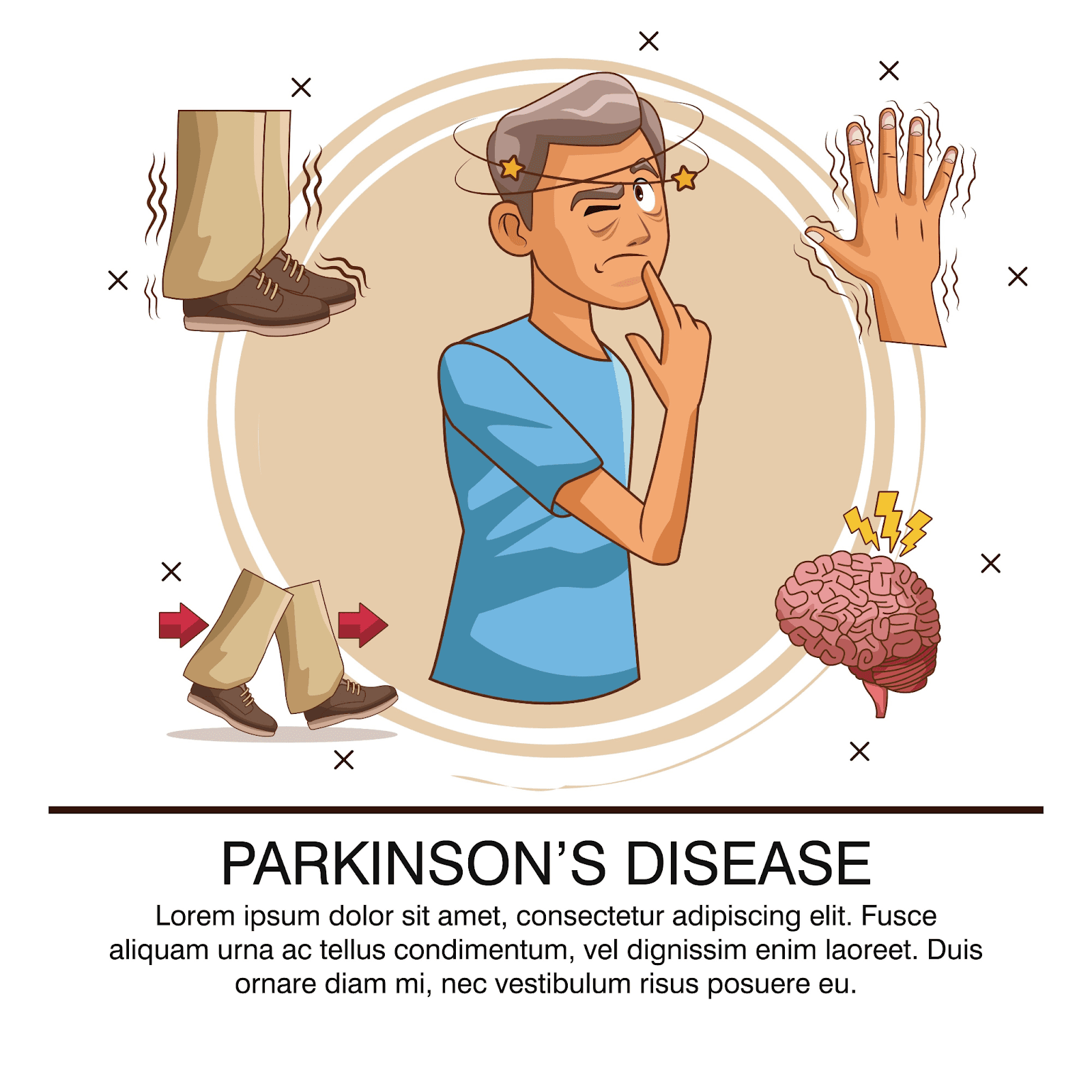
The Cardinal Symptoms (TRAP)
Neurologists look for the presence of at least two of the four primary symptoms for a diagnosis.
T - Tremor: Usually a "resting tremor" that happens when the limb is relaxed, often described as "pill-rolling" with the thumb and forefinger.
R - Rigidity: Stiffness in the limbs or trunk. The doctor may feel "cogwheel rigidity" (a ratchet-like stop-and-go movement) when moving the patient's arm.
A - Akinesia / Bradykinesia: Slowness of movement. This is often tested by asking the patient to tap their fingers quickly or stomp their foot.
P - Postural Instability: Impaired balance and coordination, often leading to falls. (This usually appears in later stages).
Here is an infographic summarizing the key symptoms of Parkinson's Disease:
The Diagnostic Process
1. Medical History
The doctor will ask about:
When symptoms started.
Family history of neurological disorders.
Exposure to toxins (pesticides, heavy metals).
Current medications (some drugs can cause Parkinson-like symptoms).
2. Physical and Neurological Exam
Observation: Checking for reduced facial expression (masked face), soft voice, or lack of arm swing while walking.
Motor Tests: Assessing muscle tone, agility, and balance.
3. Response to Medication
A significant improvement in symptoms after taking Levodopa (a dopamine replacement drug) is a strong indicator of Parkinson's Disease. This is often formalized as a "Levodopa Challenge Test."
4. Imaging Tests
MRI / CT Scan: These are mainly used to rule out other causes like strokes, tumors, or hydrocephalus. Normal PD brains often look normal on these scans.
DaTscan: A specialized imaging test that visualizes the dopamine transporter system in the brain. It can distinguish between Essential Tremor and Parkinsonian syndromes but cannot differentiate between PD and atypical parkinsonism (like MSA or PSP).
Early Warning Signs
Diagnosis often happens after motor symptoms appear, but non-motor signs can precede them by years:
Loss of smell (Anosmia).
REM Sleep Behavior Disorder: Acting out dreams, kicking, or punching while asleep.
Constipation.
Small handwriting (Micrographia).
Key Takeaways
No single test: Diagnosis is a combination of history, exam, and observation.
Expertise matters: A Movement Disorder Specialist (a type of neurologist) is best equipped to make an accurate diagnosis.
It takes time: Sometimes a diagnosis is "Probable Parkinson's" until the disease progresses or responds to medication.
Rule out others: It's crucial to ensure symptoms aren't caused by medication side effects or other neurological conditions.
FAQ
Q: Can stress cause Parkinson's?
A: Stress doesn't cause Parkinson's, but it can make symptoms like tremors temporarily worse.
Q: Is Parkinson's genetic?
A: In most cases (about 85-90%), it is not directly inherited. However, having a close relative with PD slightly increases the risk.
Q: What is the difference between Essential Tremor and Parkinson's?
A: Essential Tremor usually happens during action (like holding a cup), while Parkinson's tremor happens when the hand is at rest.
Diagnosing Parkinson’s Disease (PD) is a clinical process, meaning there is no single lab test or scan that can confirm it 100%. Neurologists rely on a detailed medical history and a physical examination to look for the cardinal signs: tremor, slowness of movement (bradykinesia), and muscle stiffness (rigidity). Specialized tests like the Levodopa Challenge Test or DaTscan (Dopamine transporter scan) may be used to support the diagnosis and rule out other conditions.
The Puzzle of Diagnosis
Parkinson's Disease cannot be identified by a simple blood draw. It is a "diagnosis of exclusion," meaning doctors must rule out other conditions that mimic PD symptoms before confirming the diagnosis. This process can sometimes take time, as symptoms often develop slowly.
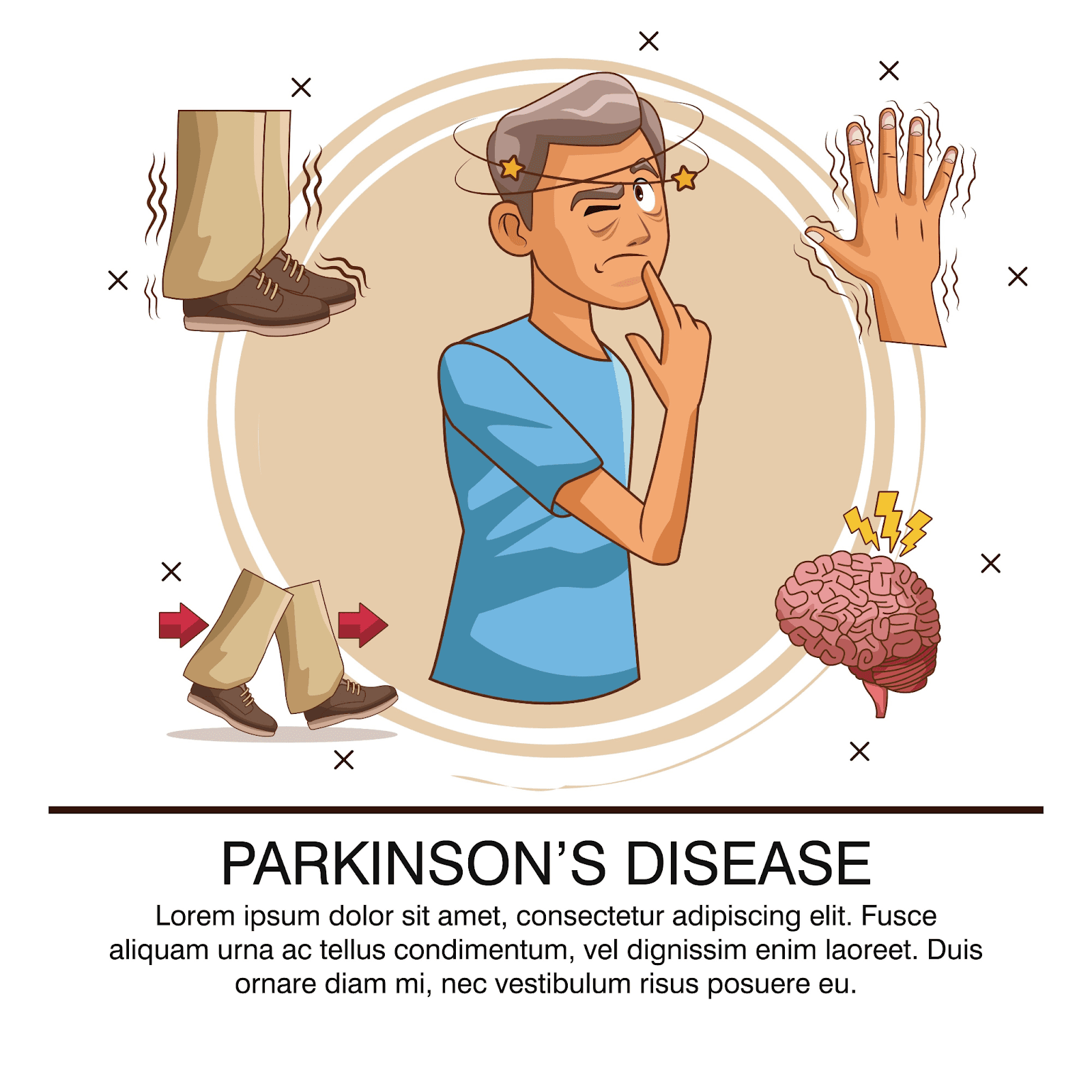
The Cardinal Symptoms (TRAP)
Neurologists look for the presence of at least two of the four primary symptoms for a diagnosis.
T - Tremor: Usually a "resting tremor" that happens when the limb is relaxed, often described as "pill-rolling" with the thumb and forefinger.
R - Rigidity: Stiffness in the limbs or trunk. The doctor may feel "cogwheel rigidity" (a ratchet-like stop-and-go movement) when moving the patient's arm.
A - Akinesia / Bradykinesia: Slowness of movement. This is often tested by asking the patient to tap their fingers quickly or stomp their foot.
P - Postural Instability: Impaired balance and coordination, often leading to falls. (This usually appears in later stages).
Here is an infographic summarizing the key symptoms of Parkinson's Disease:
The Diagnostic Process
1. Medical History
The doctor will ask about:
When symptoms started.
Family history of neurological disorders.
Exposure to toxins (pesticides, heavy metals).
Current medications (some drugs can cause Parkinson-like symptoms).
2. Physical and Neurological Exam
Observation: Checking for reduced facial expression (masked face), soft voice, or lack of arm swing while walking.
Motor Tests: Assessing muscle tone, agility, and balance.
3. Response to Medication
A significant improvement in symptoms after taking Levodopa (a dopamine replacement drug) is a strong indicator of Parkinson's Disease. This is often formalized as a "Levodopa Challenge Test."
4. Imaging Tests
MRI / CT Scan: These are mainly used to rule out other causes like strokes, tumors, or hydrocephalus. Normal PD brains often look normal on these scans.
DaTscan: A specialized imaging test that visualizes the dopamine transporter system in the brain. It can distinguish between Essential Tremor and Parkinsonian syndromes but cannot differentiate between PD and atypical parkinsonism (like MSA or PSP).
Early Warning Signs
Diagnosis often happens after motor symptoms appear, but non-motor signs can precede them by years:
Loss of smell (Anosmia).
REM Sleep Behavior Disorder: Acting out dreams, kicking, or punching while asleep.
Constipation.
Small handwriting (Micrographia).
Key Takeaways
No single test: Diagnosis is a combination of history, exam, and observation.
Expertise matters: A Movement Disorder Specialist (a type of neurologist) is best equipped to make an accurate diagnosis.
It takes time: Sometimes a diagnosis is "Probable Parkinson's" until the disease progresses or responds to medication.
Rule out others: It's crucial to ensure symptoms aren't caused by medication side effects or other neurological conditions.
FAQ
Q: Can stress cause Parkinson's?
A: Stress doesn't cause Parkinson's, but it can make symptoms like tremors temporarily worse.
Q: Is Parkinson's genetic?
A: In most cases (about 85-90%), it is not directly inherited. However, having a close relative with PD slightly increases the risk.
Q: What is the difference between Essential Tremor and Parkinson's?
A: Essential Tremor usually happens during action (like holding a cup), while Parkinson's tremor happens when the hand is at rest.

