Rehabilitation in Parkinson’s Disease: PT, OT & Speech Therapy Explained


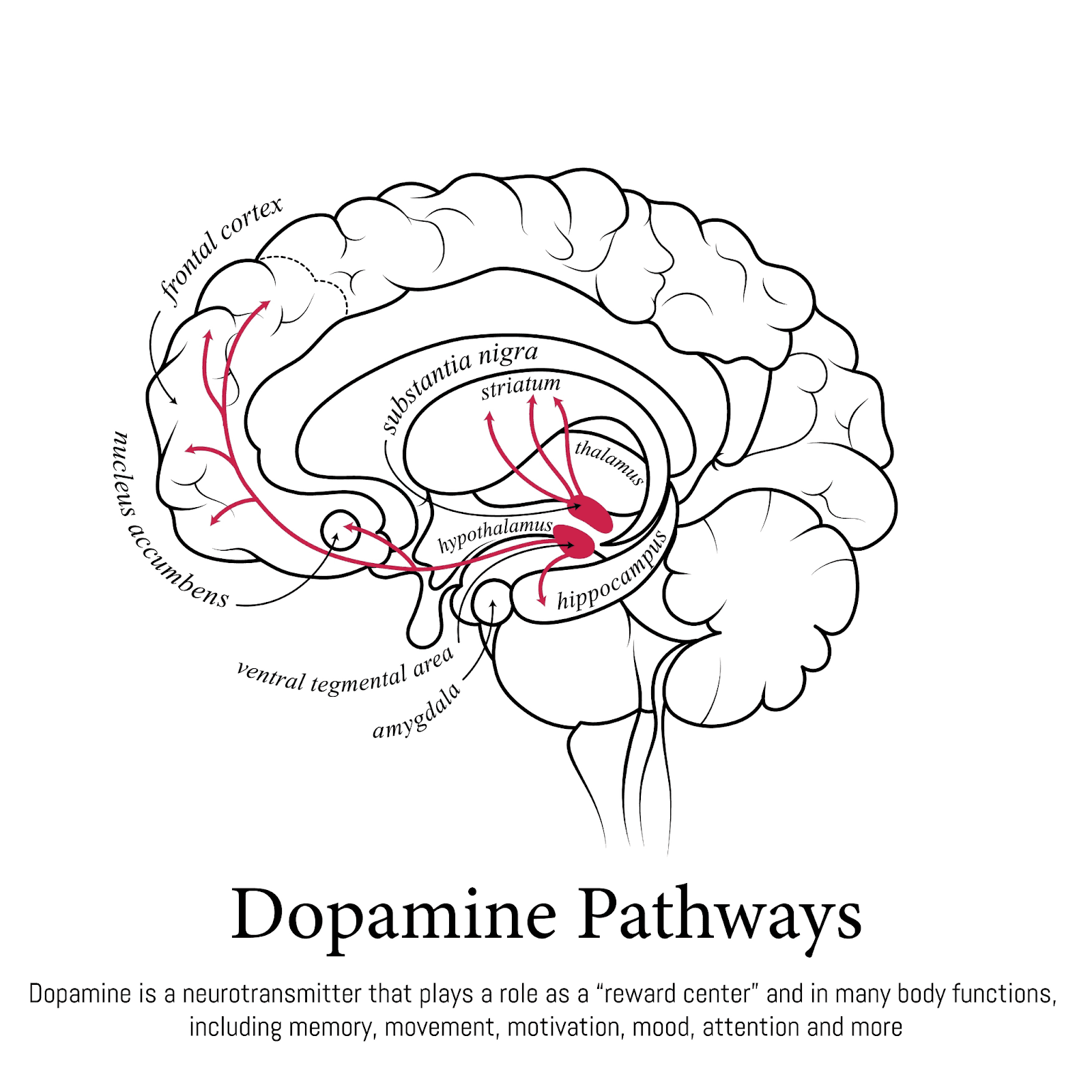
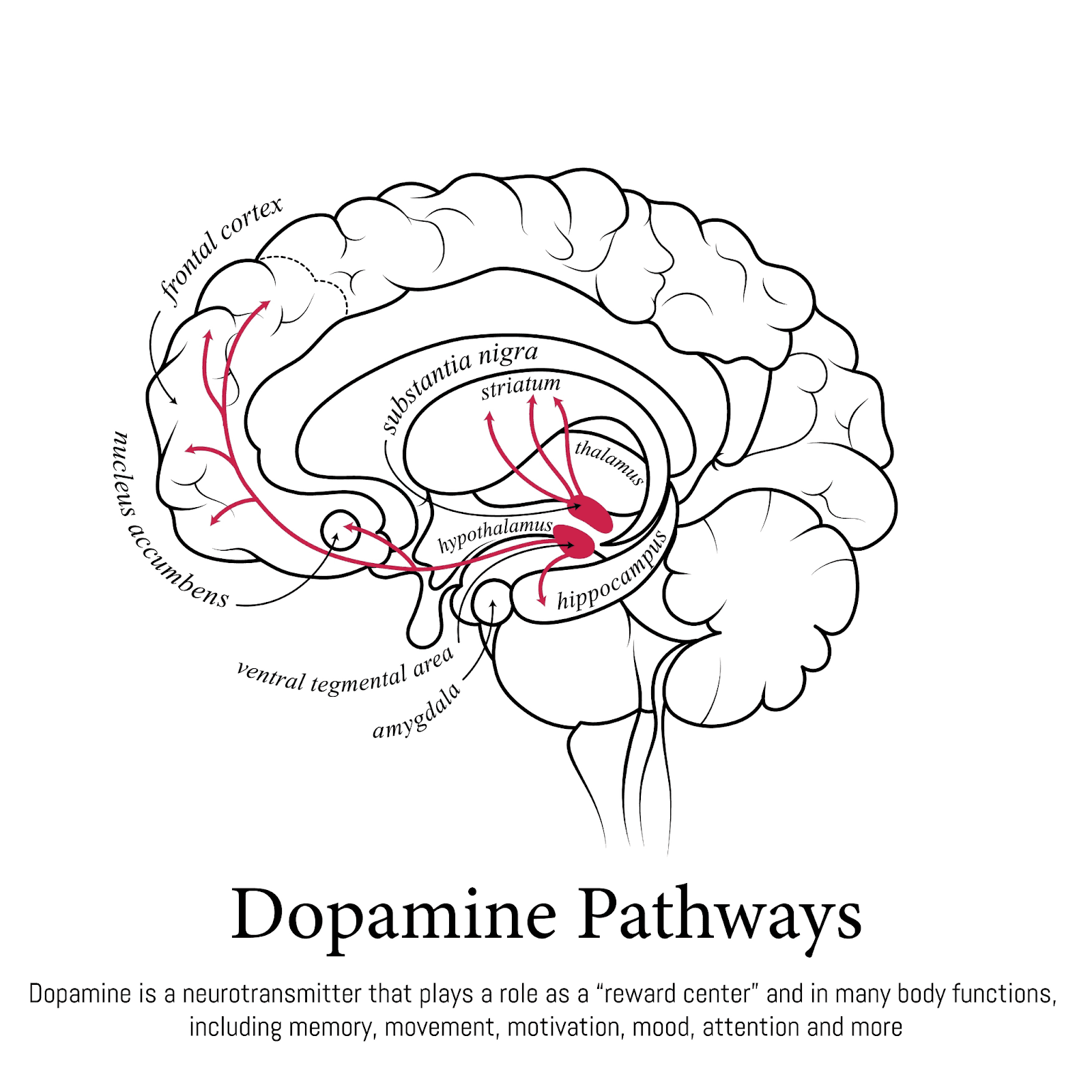
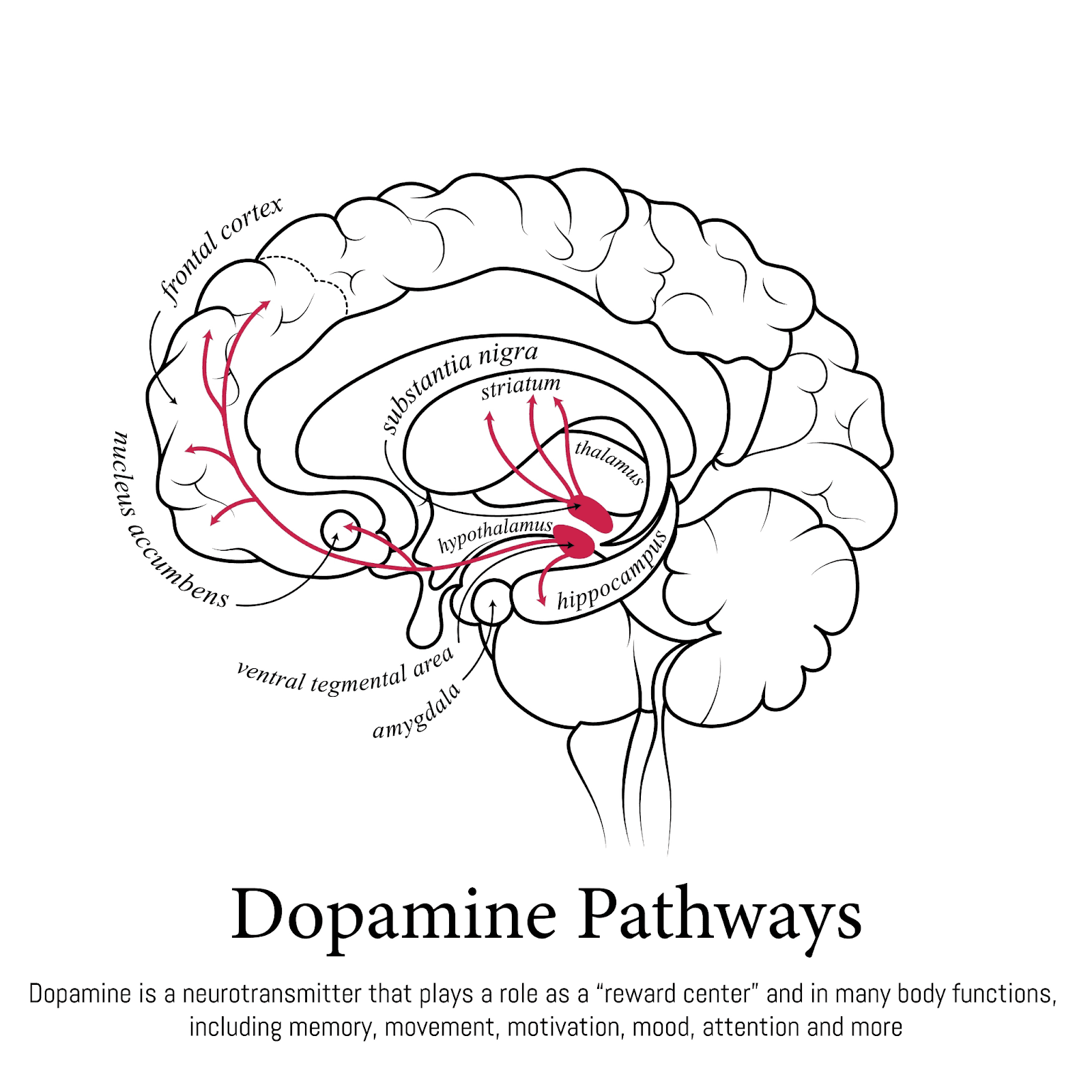
Rehabilitation is not just an "add-on" for Parkinson’s Disease (PD); it is as vital as medication. While drugs replace dopamine, rehabilitation trains the brain to use it efficiently. A comprehensive rehab program—including Physical Therapy (PT), Occupational Therapy (OT), and Speech Therapy (ST)—helps maintain independence, prevent falls, improve communication, and slow the progression of disability. The key is to start early, right after diagnosis.
Medicine + Movement = Management
For decades, the focus of PD treatment was purely pharmacological. Today, we know that neuroplasticity (the brain's ability to rewire itself) is possible even in Parkinson's. Rehabilitation drives this neuroplasticity.
The Three Pillars of Rehab
1. Physical Therapy (PT) - "The Movers"
Goal: Improve gait, balance, and flexibility.
Key Techniques:
LSVT BIG: Training patients to use large, exaggerated movements to counteract the "shrinkage" of PD.
Cueing: Using rhythmic beats or visual lines to overcome freezing of gait.
Aerobic Exercise: High-intensity exercise (like treadmill training or boxing) has been shown to protect brain cells (neuroprotection).
2. Occupational Therapy (OT) - "The Doers"
Goal: Maintain independence in daily life.
Focus Areas:
Fine Motor Skills: Buttoning shirts, handwriting, using utensils.
Home Modification: Installing grab bars, removing rugs, and rearranging the kitchen for safety.
Cognitive Strategies: Helping with planning and multitasking.
3. Speech and Language Therapy (ST) - "The Communicators"
Goal: Improve voice volume and swallowing safety.
Key Techniques:
LSVT LOUD: Training patients to "speak loud" to be heard.
Swallowing Therapy: Exercises to strengthen throat muscles and prevent aspiration pneumonia.
When to Start? The "Pre-hab" Concept
Traditionally, rehab started only after a fall or injury. The new standard is "Pre-hab"—starting therapy immediately upon diagnosis.
Baseline Assessment: Establishing a baseline for movement and voice.
Prevention: Learning correct movement patterns before bad habits set in.
Delaying Disability: Early exercise can delay the onset of severe symptoms.
The Role of Specialized Centers
Centers like the Newro Rehabilitation Centre (led by Dr. Sharan Srinivasan) offer multidisciplinary care under one roof. This integrated approach ensures that the PT knows what the OT is doing, and the neurologist adjusts meds to support the therapy sessions.
Key Takeaways
Exercise is medicine: It is the only thing proven to potentially slow disease progression.
Consistency is key: Going to therapy once a week isn't enough. You must do the homework exercises daily.
It's never too late: Even advanced patients can benefit from assisted movement and positioning to reduce pain.
Family involvement: Caregivers learn how to safely help their loved ones move, reducing the risk of injury for both.
FAQ
Q: Does insurance cover rehab?
A: Most insurance plans cover PT, OT, and ST if prescribed by a doctor. However, maintenance therapy (ongoing sessions) may have limits.
Q: Can I just join a gym?
A: General exercise is great, but a PD-specialized therapist can teach you specific strategies (like how to stop a freeze) that a personal trainer cannot.
Q: What is Rock Steady Boxing?A: It is a non-contact boxing program specifically designed for PD. It improves balance, hand-eye coordination, and agility.
Rehabilitation is not just an "add-on" for Parkinson’s Disease (PD); it is as vital as medication. While drugs replace dopamine, rehabilitation trains the brain to use it efficiently. A comprehensive rehab program—including Physical Therapy (PT), Occupational Therapy (OT), and Speech Therapy (ST)—helps maintain independence, prevent falls, improve communication, and slow the progression of disability. The key is to start early, right after diagnosis.
Medicine + Movement = Management
For decades, the focus of PD treatment was purely pharmacological. Today, we know that neuroplasticity (the brain's ability to rewire itself) is possible even in Parkinson's. Rehabilitation drives this neuroplasticity.
The Three Pillars of Rehab
1. Physical Therapy (PT) - "The Movers"
Goal: Improve gait, balance, and flexibility.
Key Techniques:
LSVT BIG: Training patients to use large, exaggerated movements to counteract the "shrinkage" of PD.
Cueing: Using rhythmic beats or visual lines to overcome freezing of gait.
Aerobic Exercise: High-intensity exercise (like treadmill training or boxing) has been shown to protect brain cells (neuroprotection).
2. Occupational Therapy (OT) - "The Doers"
Goal: Maintain independence in daily life.
Focus Areas:
Fine Motor Skills: Buttoning shirts, handwriting, using utensils.
Home Modification: Installing grab bars, removing rugs, and rearranging the kitchen for safety.
Cognitive Strategies: Helping with planning and multitasking.
3. Speech and Language Therapy (ST) - "The Communicators"
Goal: Improve voice volume and swallowing safety.
Key Techniques:
LSVT LOUD: Training patients to "speak loud" to be heard.
Swallowing Therapy: Exercises to strengthen throat muscles and prevent aspiration pneumonia.
When to Start? The "Pre-hab" Concept
Traditionally, rehab started only after a fall or injury. The new standard is "Pre-hab"—starting therapy immediately upon diagnosis.
Baseline Assessment: Establishing a baseline for movement and voice.
Prevention: Learning correct movement patterns before bad habits set in.
Delaying Disability: Early exercise can delay the onset of severe symptoms.
The Role of Specialized Centers
Centers like the Newro Rehabilitation Centre (led by Dr. Sharan Srinivasan) offer multidisciplinary care under one roof. This integrated approach ensures that the PT knows what the OT is doing, and the neurologist adjusts meds to support the therapy sessions.
Key Takeaways
Exercise is medicine: It is the only thing proven to potentially slow disease progression.
Consistency is key: Going to therapy once a week isn't enough. You must do the homework exercises daily.
It's never too late: Even advanced patients can benefit from assisted movement and positioning to reduce pain.
Family involvement: Caregivers learn how to safely help their loved ones move, reducing the risk of injury for both.
FAQ
Q: Does insurance cover rehab?
A: Most insurance plans cover PT, OT, and ST if prescribed by a doctor. However, maintenance therapy (ongoing sessions) may have limits.
Q: Can I just join a gym?
A: General exercise is great, but a PD-specialized therapist can teach you specific strategies (like how to stop a freeze) that a personal trainer cannot.
Q: What is Rock Steady Boxing?A: It is a non-contact boxing program specifically designed for PD. It improves balance, hand-eye coordination, and agility.
Rehabilitation is not just an "add-on" for Parkinson’s Disease (PD); it is as vital as medication. While drugs replace dopamine, rehabilitation trains the brain to use it efficiently. A comprehensive rehab program—including Physical Therapy (PT), Occupational Therapy (OT), and Speech Therapy (ST)—helps maintain independence, prevent falls, improve communication, and slow the progression of disability. The key is to start early, right after diagnosis.
Medicine + Movement = Management
For decades, the focus of PD treatment was purely pharmacological. Today, we know that neuroplasticity (the brain's ability to rewire itself) is possible even in Parkinson's. Rehabilitation drives this neuroplasticity.
The Three Pillars of Rehab
1. Physical Therapy (PT) - "The Movers"
Goal: Improve gait, balance, and flexibility.
Key Techniques:
LSVT BIG: Training patients to use large, exaggerated movements to counteract the "shrinkage" of PD.
Cueing: Using rhythmic beats or visual lines to overcome freezing of gait.
Aerobic Exercise: High-intensity exercise (like treadmill training or boxing) has been shown to protect brain cells (neuroprotection).
2. Occupational Therapy (OT) - "The Doers"
Goal: Maintain independence in daily life.
Focus Areas:
Fine Motor Skills: Buttoning shirts, handwriting, using utensils.
Home Modification: Installing grab bars, removing rugs, and rearranging the kitchen for safety.
Cognitive Strategies: Helping with planning and multitasking.
3. Speech and Language Therapy (ST) - "The Communicators"
Goal: Improve voice volume and swallowing safety.
Key Techniques:
LSVT LOUD: Training patients to "speak loud" to be heard.
Swallowing Therapy: Exercises to strengthen throat muscles and prevent aspiration pneumonia.
When to Start? The "Pre-hab" Concept
Traditionally, rehab started only after a fall or injury. The new standard is "Pre-hab"—starting therapy immediately upon diagnosis.
Baseline Assessment: Establishing a baseline for movement and voice.
Prevention: Learning correct movement patterns before bad habits set in.
Delaying Disability: Early exercise can delay the onset of severe symptoms.
The Role of Specialized Centers
Centers like the Newro Rehabilitation Centre (led by Dr. Sharan Srinivasan) offer multidisciplinary care under one roof. This integrated approach ensures that the PT knows what the OT is doing, and the neurologist adjusts meds to support the therapy sessions.
Key Takeaways
Exercise is medicine: It is the only thing proven to potentially slow disease progression.
Consistency is key: Going to therapy once a week isn't enough. You must do the homework exercises daily.
It's never too late: Even advanced patients can benefit from assisted movement and positioning to reduce pain.
Family involvement: Caregivers learn how to safely help their loved ones move, reducing the risk of injury for both.
FAQ
Q: Does insurance cover rehab?
A: Most insurance plans cover PT, OT, and ST if prescribed by a doctor. However, maintenance therapy (ongoing sessions) may have limits.
Q: Can I just join a gym?
A: General exercise is great, but a PD-specialized therapist can teach you specific strategies (like how to stop a freeze) that a personal trainer cannot.
Q: What is Rock Steady Boxing?A: It is a non-contact boxing program specifically designed for PD. It improves balance, hand-eye coordination, and agility.

