Bradykinesia in Parkinson’s Disease: Symptoms, Causes & Treatment


Bradykinesia, meaning "slow movement," is the hallmark symptom of Parkinson’s Disease (PD). A diagnosis of PD cannot be made without it. It is not just about moving slowly; it involves a difficulty in initiating movement and a decrease in the amplitude (size) of movement. From a masked face to a shuffling walk and small handwriting, bradykinesia affects almost every physical action and is often the most disabling symptom for patients.
The Slowing Down of Life
Imagine wearing a heavy suit of armor while trying to move through water. That is often how patients describe bradykinesia. It is caused by the brain's failure to send the "GO" signal to the muscles with enough force.
Here’s a visual representation of how a healthy brain sends "go" signals compared to a brain affected by Parkinson's:
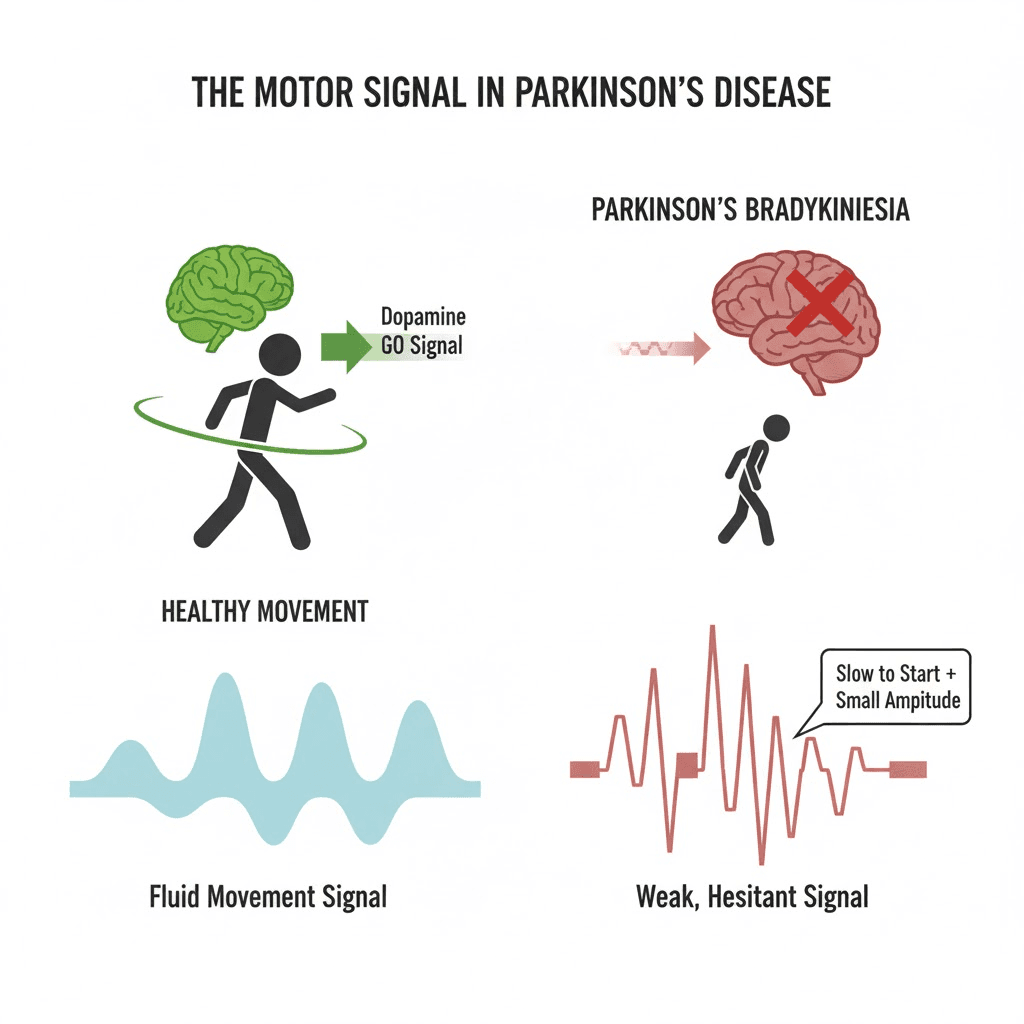
How Bradykinesia Manifests
1. General Slowness
Everything takes longer: getting dressed, eating, showering. This requires significant patience from both the patient and the caregiver.
2. Difficulty Initiating Movement (Akinesia)
Hesitation: The brain knows what to do, but the body won't start. This is often seen when trying to get out of a chair or start walking.
3. Reduced Amplitude (Hypokinesia)
Micrographia: Handwriting starts normal but gets smaller and smaller across the page.
Shuffling Gait: Steps become short and dragging.
Soft Voice (Hypophonia): The voice becomes quiet and monotone because the chest muscles aren't pumping enough air.
4. Loss of Automatic Movements
Blinking: Reduced blinking leads to dry eyes and the "stare" of Parkinson's.
Arm Swing: Walking without the natural arm swing.
Swallowing: Reduced automatic swallowing leads to drooling.
The Sequence Effect
Bradykinesia is characterized by a progressive reduction in speed and amplitude during repetitive actions. If you ask a patient to tap their finger and thumb together repeatedly, the taps will get slower and smaller until they barely touch. This is a key test neurologists use for diagnosis.
Management Strategies
1. Medication
Levodopa: This is the gold standard. It replenishes dopamine and directly improves speed and amplitude. When the medication wears off ("OFF" time), bradykinesia returns immediately.
2. Cueing Strategies (Tricking the Brain)
Since the automatic movement center is broken, patients can use the conscious part of their brain to bypass the block.
Visual Cues: Stepping over a laser line or a strip of tape on the floor.
Auditory Cues: Walking to the beat of a metronome or rhythmic music.
Verbal Cues: Counting "One, Two, One, Two" out loud while walking.
3. LSVT BIG Therapy
This is a specialized physical therapy program that trains patients to "Think BIG." By consciously over-exaggerating movements (taking giant steps, throwing arms wide), the patient ends up moving normally.
Key Takeaways
It's not laziness: The patient is trying hard, often working twice as hard as a healthy person to do the same task.
Patience is vital: Rushing a patient usually causes stress, which freezes them up further.
Safety: Slowness in reacting (like catching oneself after a trip) increases the risk of injury.
Keep the voice loud: Just like movement, the voice needs exercise. Singing and reading aloud help fight vocal bradykinesia.
FAQ
Q: Is bradykinesia the same as fatigue?
A: No, but they are related. Moving slowly requires more energy, so patients with bradykinesia get tired faster.
Q: Can it be reversed?
A: Medication can significantly reverse it for many years. Exercise helps maintain the gains.
Q: Why do I freeze in doorways?
A: This is a severe form of bradykinesia/akinesia. The visual clutter of the doorframe confuses the brain's motor planning.
Bradykinesia, meaning "slow movement," is the hallmark symptom of Parkinson’s Disease (PD). A diagnosis of PD cannot be made without it. It is not just about moving slowly; it involves a difficulty in initiating movement and a decrease in the amplitude (size) of movement. From a masked face to a shuffling walk and small handwriting, bradykinesia affects almost every physical action and is often the most disabling symptom for patients.
The Slowing Down of Life
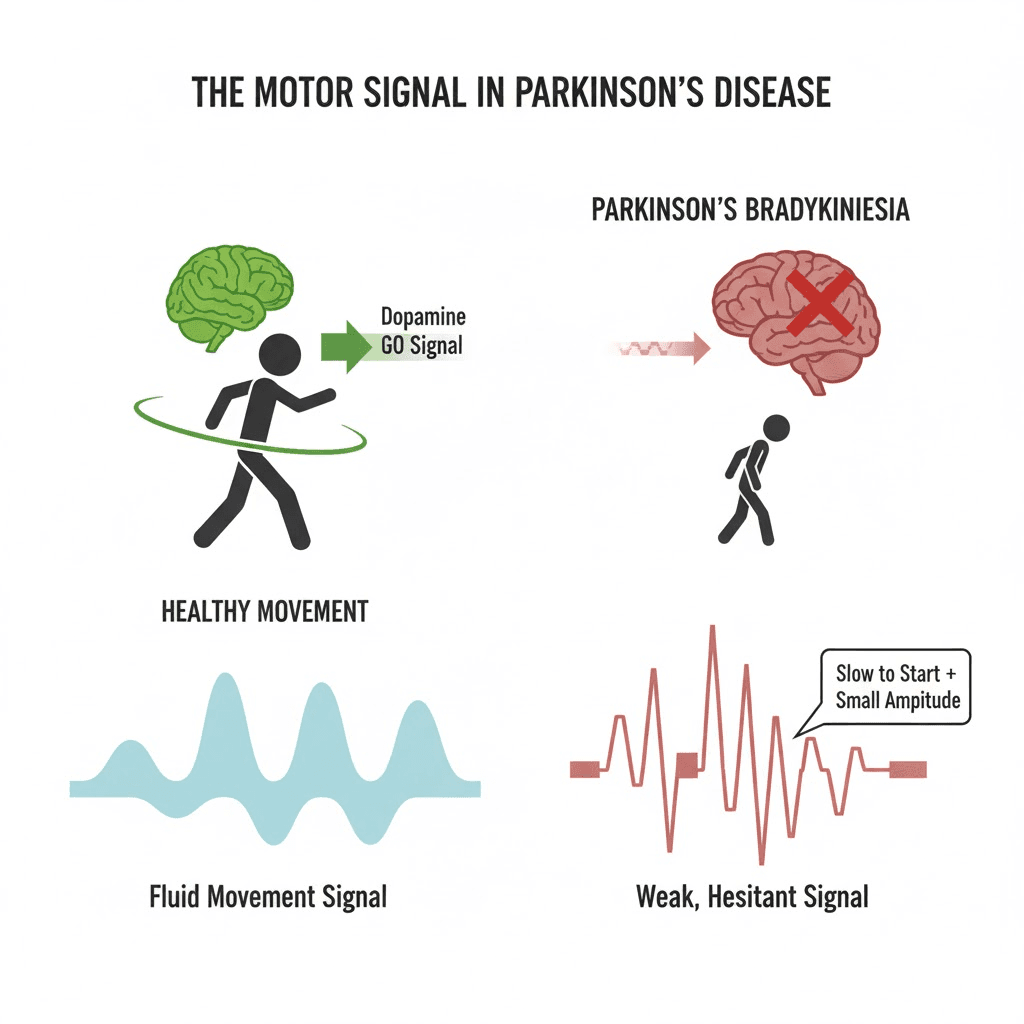
Imagine wearing a heavy suit of armor while trying to move through water. That is often how patients describe bradykinesia. It is caused by the brain's failure to send the "GO" signal to the muscles with enough force.
Here’s a visual representation of how a healthy brain sends "go" signals compared to a brain affected by Parkinson's:
How Bradykinesia Manifests
1. General Slowness
Everything takes longer: getting dressed, eating, showering. This requires significant patience from both the patient and the caregiver.
2. Difficulty Initiating Movement (Akinesia)
Hesitation: The brain knows what to do, but the body won't start. This is often seen when trying to get out of a chair or start walking.
3. Reduced Amplitude (Hypokinesia)
Micrographia: Handwriting starts normal but gets smaller and smaller across the page.
Shuffling Gait: Steps become short and dragging.
Soft Voice (Hypophonia): The voice becomes quiet and monotone because the chest muscles aren't pumping enough air.
4. Loss of Automatic Movements
Blinking: Reduced blinking leads to dry eyes and the "stare" of Parkinson's.
Arm Swing: Walking without the natural arm swing.
Swallowing: Reduced automatic swallowing leads to drooling.
The Sequence Effect
Bradykinesia is characterized by a progressive reduction in speed and amplitude during repetitive actions. If you ask a patient to tap their finger and thumb together repeatedly, the taps will get slower and smaller until they barely touch. This is a key test neurologists use for diagnosis.
Management Strategies
1. Medication
Levodopa: This is the gold standard. It replenishes dopamine and directly improves speed and amplitude. When the medication wears off ("OFF" time), bradykinesia returns immediately.
2. Cueing Strategies (Tricking the Brain)
Since the automatic movement center is broken, patients can use the conscious part of their brain to bypass the block.
Visual Cues: Stepping over a laser line or a strip of tape on the floor.
Auditory Cues: Walking to the beat of a metronome or rhythmic music.
Verbal Cues: Counting "One, Two, One, Two" out loud while walking.
3. LSVT BIG Therapy
This is a specialized physical therapy program that trains patients to "Think BIG." By consciously over-exaggerating movements (taking giant steps, throwing arms wide), the patient ends up moving normally.
Key Takeaways
It's not laziness: The patient is trying hard, often working twice as hard as a healthy person to do the same task.
Patience is vital: Rushing a patient usually causes stress, which freezes them up further.
Safety: Slowness in reacting (like catching oneself after a trip) increases the risk of injury.
Keep the voice loud: Just like movement, the voice needs exercise. Singing and reading aloud help fight vocal bradykinesia.
FAQ
Q: Is bradykinesia the same as fatigue?
A: No, but they are related. Moving slowly requires more energy, so patients with bradykinesia get tired faster.
Q: Can it be reversed?
A: Medication can significantly reverse it for many years. Exercise helps maintain the gains.
Q: Why do I freeze in doorways?
A: This is a severe form of bradykinesia/akinesia. The visual clutter of the doorframe confuses the brain's motor planning.
Bradykinesia, meaning "slow movement," is the hallmark symptom of Parkinson’s Disease (PD). A diagnosis of PD cannot be made without it. It is not just about moving slowly; it involves a difficulty in initiating movement and a decrease in the amplitude (size) of movement. From a masked face to a shuffling walk and small handwriting, bradykinesia affects almost every physical action and is often the most disabling symptom for patients.
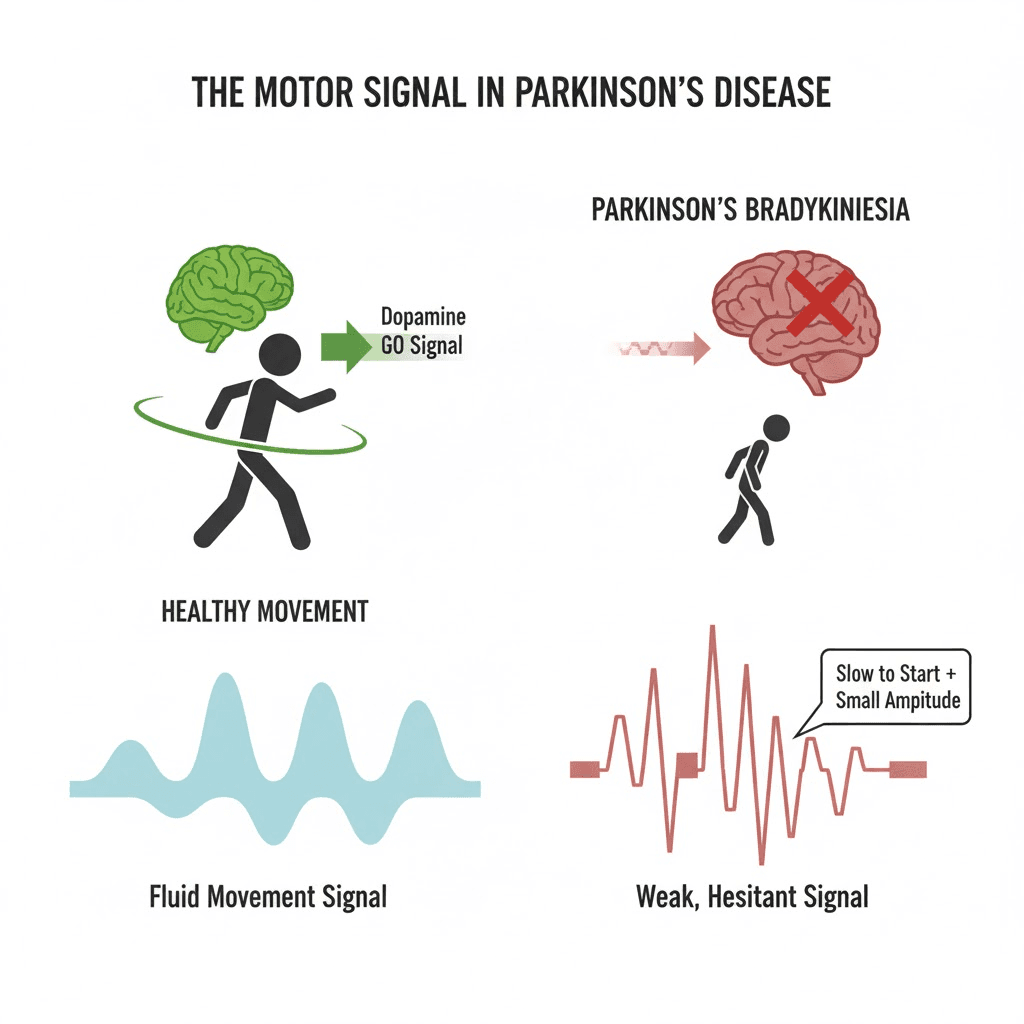
The Slowing Down of Life
Imagine wearing a heavy suit of armor while trying to move through water. That is often how patients describe bradykinesia. It is caused by the brain's failure to send the "GO" signal to the muscles with enough force.
Here’s a visual representation of how a healthy brain sends "go" signals compared to a brain affected by Parkinson's:
How Bradykinesia Manifests
1. General Slowness
Everything takes longer: getting dressed, eating, showering. This requires significant patience from both the patient and the caregiver.
2. Difficulty Initiating Movement (Akinesia)
Hesitation: The brain knows what to do, but the body won't start. This is often seen when trying to get out of a chair or start walking.
3. Reduced Amplitude (Hypokinesia)
Micrographia: Handwriting starts normal but gets smaller and smaller across the page.
Shuffling Gait: Steps become short and dragging.
Soft Voice (Hypophonia): The voice becomes quiet and monotone because the chest muscles aren't pumping enough air.
4. Loss of Automatic Movements
Blinking: Reduced blinking leads to dry eyes and the "stare" of Parkinson's.
Arm Swing: Walking without the natural arm swing.
Swallowing: Reduced automatic swallowing leads to drooling.
The Sequence Effect
Bradykinesia is characterized by a progressive reduction in speed and amplitude during repetitive actions. If you ask a patient to tap their finger and thumb together repeatedly, the taps will get slower and smaller until they barely touch. This is a key test neurologists use for diagnosis.
Management Strategies
1. Medication
Levodopa: This is the gold standard. It replenishes dopamine and directly improves speed and amplitude. When the medication wears off ("OFF" time), bradykinesia returns immediately.
2. Cueing Strategies (Tricking the Brain)
Since the automatic movement center is broken, patients can use the conscious part of their brain to bypass the block.
Visual Cues: Stepping over a laser line or a strip of tape on the floor.
Auditory Cues: Walking to the beat of a metronome or rhythmic music.
Verbal Cues: Counting "One, Two, One, Two" out loud while walking.
3. LSVT BIG Therapy
This is a specialized physical therapy program that trains patients to "Think BIG." By consciously over-exaggerating movements (taking giant steps, throwing arms wide), the patient ends up moving normally.
Key Takeaways
It's not laziness: The patient is trying hard, often working twice as hard as a healthy person to do the same task.
Patience is vital: Rushing a patient usually causes stress, which freezes them up further.
Safety: Slowness in reacting (like catching oneself after a trip) increases the risk of injury.
Keep the voice loud: Just like movement, the voice needs exercise. Singing and reading aloud help fight vocal bradykinesia.
FAQ
Q: Is bradykinesia the same as fatigue?
A: No, but they are related. Moving slowly requires more energy, so patients with bradykinesia get tired faster.
Q: Can it be reversed?
A: Medication can significantly reverse it for many years. Exercise helps maintain the gains.
Q: Why do I freeze in doorways?
A: This is a severe form of bradykinesia/akinesia. The visual clutter of the doorframe confuses the brain's motor planning.

