Parkinson’s Disease and Its Variants


Parkinson’s Disease (PD) is a progressive neurodegenerative disorder affecting movement, but it is not the only condition with these symptoms. "Parkinsonism" is an umbrella term for a group of disorders that share features like tremors, rigidity, and slow movement. These variants, such as Multiple System Atrophy (MSA) and Progressive Supranuclear Palsy (PSP), often progress faster than typical PD and respond differently to medication. Accurate diagnosis is crucial for effective management.
Beyond Typical Parkinson's
When we hear "Parkinson's," we often think of the classic shaking palsy described by James Parkinson. However, many patients present with symptoms that look like Parkinson's but do not follow the typical course. These are often referred to as Atypical Parkinsonism or Parkinson-Plus Syndromes.
Idiopathic Parkinson’s Disease
This is the most common form. "Idiopathic" means the cause is unknown.
Key Features: Resting tremor, rigidity, bradykinesia (slowness), and postural instability.
Response to Meds: Usually responds well to Levodopa.
Progression: Generally slow and gradual.
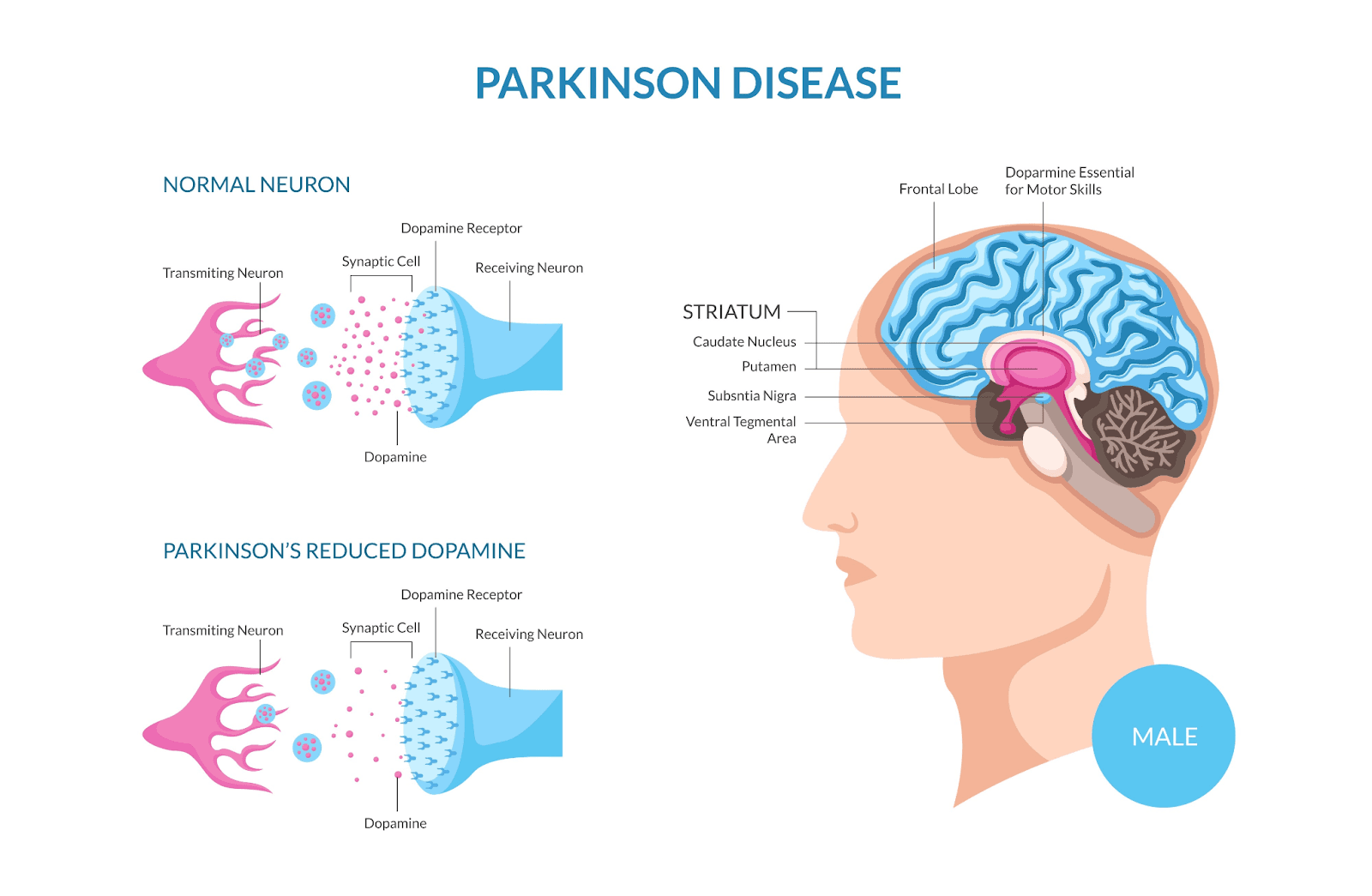
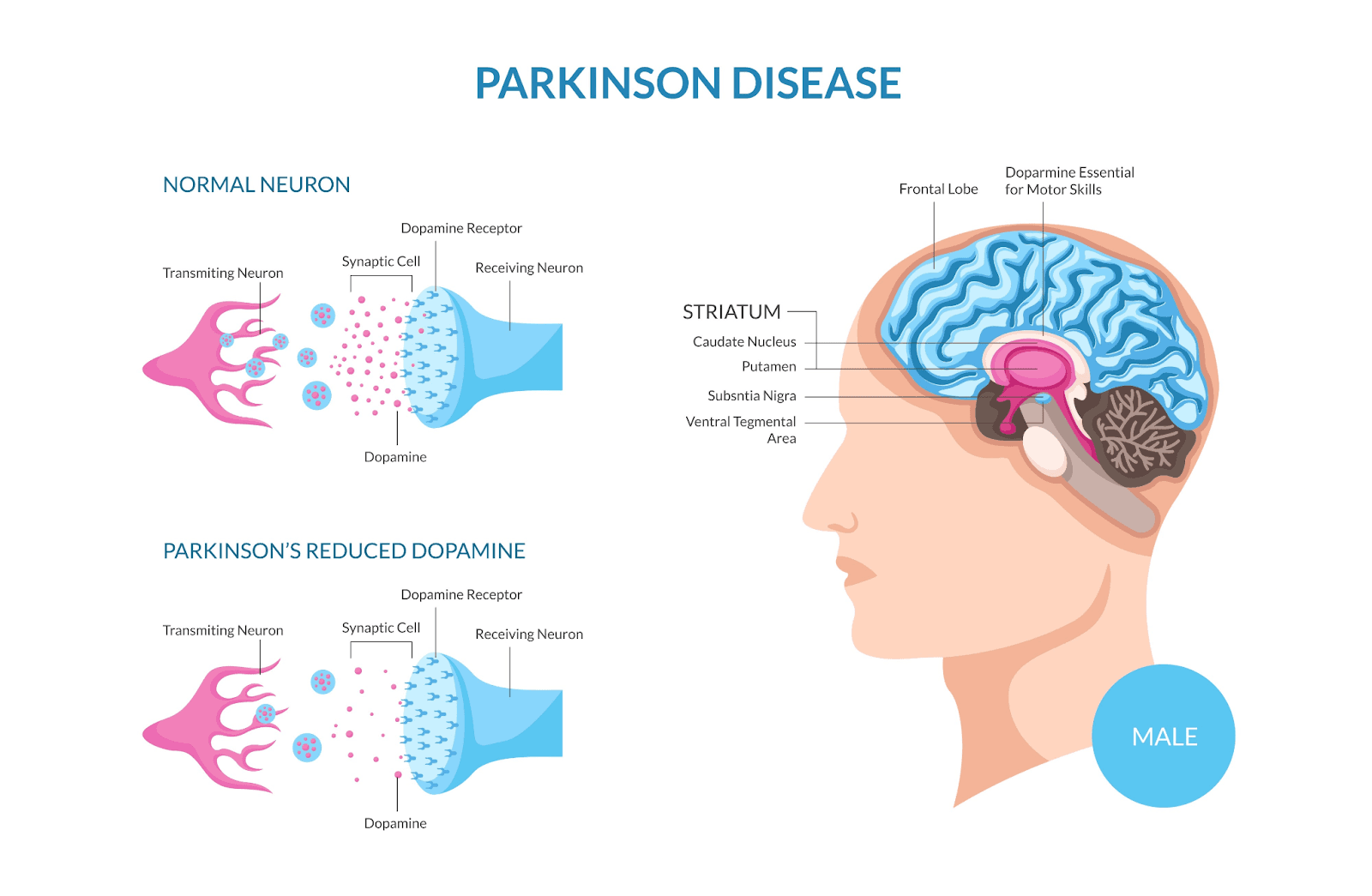
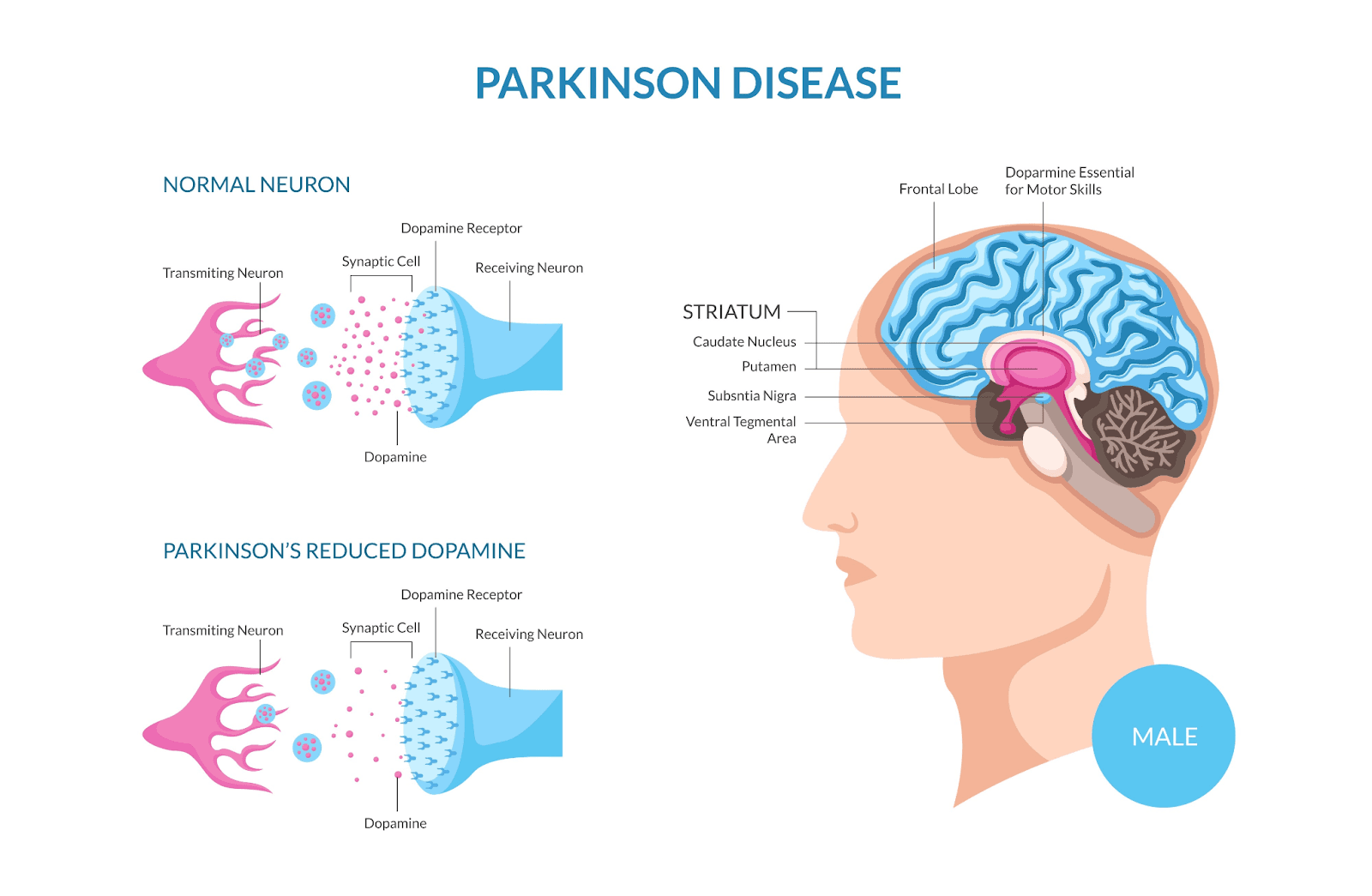
This illustration highlights the biological basis of Parkinson's, showing the reduction of dopamine in the brain:
The Variants (Atypical Parkinsonism)
These conditions mimic PD but involve damage to different parts of the brain and often have additional symptoms.
1. Multiple System Atrophy (MSA)
MSA affects the autonomic nervous system, which controls involuntary actions like blood pressure, digestion etc.
Symptoms: Fainting spells (orthostatic hypotension), bladder control issues, and speech difficulties alongside stiffness.
Prognosis: Progresses more rapidly than typical PD.
2. Progressive Supranuclear Palsy (PSP)
PSP is characterized by problems with eye movements and balance.
Symptoms: Frequent falls (often backwards), difficulty looking up or down, and personality changes.
Distinction: Tremor is less common in PSP than in PD.
3. Corticobasal Degeneration (CBD)
This is a rare form that affects one side of the body more than the other.
Symptoms: "Alien limb phenomenon" (where a limb seems to move on its own), severe stiffness, and difficulty with complex movements (apraxia).
4. Lewy Body Dementia (LBD)
While PD can lead to dementia later in life, LBD presents with cognitive decline and hallucinations early in the disease course, often before or at the same time as movement issues.
5. Vascular Parkinsonism
Caused by multiple small strokes in the brain area controlling movement.
Symptoms: Often affects the legs more than the upper body ("lower body Parkinsonism"), leading to a shuffling gait.
Response to Meds: Poor response to Levodopa.
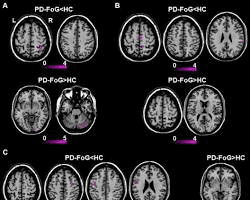
Advanced imaging, such as MRI scans, can help doctors differentiate between typical Parkinson's and its variants by looking for specific patterns of atrophy:
Why Distinction Matters
Diagnosing the correct variant is vital because:
Medication Management: Atypical forms often do not respond well to standard Parkinson's drugs like Levodopa.
Prognosis: Variants often progress faster and require different support strategies.
Symptom Management: Treatments need to target specific issues like low blood pressure in MSA or swallowing difficulties in PSP.
A thorough clinical examination by a specialist is the primary method for distinguishing between these complex disorders:

Key Takeaways
Not all tremors are Parkinson's: A thorough neurological exam is needed to rule out variants.
Watch for "Red Flags": Early falls, hallucinations, or severe blood pressure drops suggest a variant.
Medication response is a clue: If Levodopa doesn't help, it might be Atypical Parkinsonism.
Therapy is key: Regardless of the type, physical and speech therapy are essential to maintain function.
FAQ
Q: Can a blood test diagnose these variants?
A: No, there is currently no definitive blood test. Diagnosis is based on clinical history, physical exams, and sometimes MRI scans to look for specific brain atrophy patterns.
Q: Is Atypical Parkinsonism hereditary?
A: Most cases are sporadic, meaning they happen randomly. However, genetics can play a role in some rare forms.
Q: Can you have both Parkinson's and a variant?
A: It is rare to have both. Usually, it is one specific underlying pathology causing the symptoms.
Parkinson’s Disease (PD) is a progressive neurodegenerative disorder affecting movement, but it is not the only condition with these symptoms. "Parkinsonism" is an umbrella term for a group of disorders that share features like tremors, rigidity, and slow movement. These variants, such as Multiple System Atrophy (MSA) and Progressive Supranuclear Palsy (PSP), often progress faster than typical PD and respond differently to medication. Accurate diagnosis is crucial for effective management.
Beyond Typical Parkinson's
When we hear "Parkinson's," we often think of the classic shaking palsy described by James Parkinson. However, many patients present with symptoms that look like Parkinson's but do not follow the typical course. These are often referred to as Atypical Parkinsonism or Parkinson-Plus Syndromes.
Idiopathic Parkinson’s Disease
This is the most common form. "Idiopathic" means the cause is unknown.
Key Features: Resting tremor, rigidity, bradykinesia (slowness), and postural instability.
Response to Meds: Usually responds well to Levodopa.
Progression: Generally slow and gradual.
This illustration highlights the biological basis of Parkinson's, showing the reduction of dopamine in the brain:
The Variants (Atypical Parkinsonism)
These conditions mimic PD but involve damage to different parts of the brain and often have additional symptoms.
1. Multiple System Atrophy (MSA)
MSA affects the autonomic nervous system, which controls involuntary actions like blood pressure, digestion etc.
Symptoms: Fainting spells (orthostatic hypotension), bladder control issues, and speech difficulties alongside stiffness.
Prognosis: Progresses more rapidly than typical PD.
2. Progressive Supranuclear Palsy (PSP)
PSP is characterized by problems with eye movements and balance.
Symptoms: Frequent falls (often backwards), difficulty looking up or down, and personality changes.
Distinction: Tremor is less common in PSP than in PD.
3. Corticobasal Degeneration (CBD)
This is a rare form that affects one side of the body more than the other.
Symptoms: "Alien limb phenomenon" (where a limb seems to move on its own), severe stiffness, and difficulty with complex movements (apraxia).
4. Lewy Body Dementia (LBD)
While PD can lead to dementia later in life, LBD presents with cognitive decline and hallucinations early in the disease course, often before or at the same time as movement issues.
5. Vascular Parkinsonism
Caused by multiple small strokes in the brain area controlling movement.
Symptoms: Often affects the legs more than the upper body ("lower body Parkinsonism"), leading to a shuffling gait.
Response to Meds: Poor response to Levodopa.
Advanced imaging, such as MRI scans, can help doctors differentiate between typical Parkinson's and its variants by looking for specific patterns of atrophy:
Why Distinction Matters
Diagnosing the correct variant is vital because:
Medication Management: Atypical forms often do not respond well to standard Parkinson's drugs like Levodopa.
Prognosis: Variants often progress faster and require different support strategies.
Symptom Management: Treatments need to target specific issues like low blood pressure in MSA or swallowing difficulties in PSP.
A thorough clinical examination by a specialist is the primary method for distinguishing between these complex disorders:

Key Takeaways
Not all tremors are Parkinson's: A thorough neurological exam is needed to rule out variants.
Watch for "Red Flags": Early falls, hallucinations, or severe blood pressure drops suggest a variant.
Medication response is a clue: If Levodopa doesn't help, it might be Atypical Parkinsonism.
Therapy is key: Regardless of the type, physical and speech therapy are essential to maintain function.
FAQ
Q: Can a blood test diagnose these variants?
A: No, there is currently no definitive blood test. Diagnosis is based on clinical history, physical exams, and sometimes MRI scans to look for specific brain atrophy patterns.
Q: Is Atypical Parkinsonism hereditary?
A: Most cases are sporadic, meaning they happen randomly. However, genetics can play a role in some rare forms.
Q: Can you have both Parkinson's and a variant?
A: It is rare to have both. Usually, it is one specific underlying pathology causing the symptoms.
Parkinson’s Disease (PD) is a progressive neurodegenerative disorder affecting movement, but it is not the only condition with these symptoms. "Parkinsonism" is an umbrella term for a group of disorders that share features like tremors, rigidity, and slow movement. These variants, such as Multiple System Atrophy (MSA) and Progressive Supranuclear Palsy (PSP), often progress faster than typical PD and respond differently to medication. Accurate diagnosis is crucial for effective management.
Beyond Typical Parkinson's
When we hear "Parkinson's," we often think of the classic shaking palsy described by James Parkinson. However, many patients present with symptoms that look like Parkinson's but do not follow the typical course. These are often referred to as Atypical Parkinsonism or Parkinson-Plus Syndromes.
Idiopathic Parkinson’s Disease
This is the most common form. "Idiopathic" means the cause is unknown.
Key Features: Resting tremor, rigidity, bradykinesia (slowness), and postural instability.
Response to Meds: Usually responds well to Levodopa.
Progression: Generally slow and gradual.
This illustration highlights the biological basis of Parkinson's, showing the reduction of dopamine in the brain:
The Variants (Atypical Parkinsonism)
These conditions mimic PD but involve damage to different parts of the brain and often have additional symptoms.
1. Multiple System Atrophy (MSA)
MSA affects the autonomic nervous system, which controls involuntary actions like blood pressure, digestion etc.
Symptoms: Fainting spells (orthostatic hypotension), bladder control issues, and speech difficulties alongside stiffness.
Prognosis: Progresses more rapidly than typical PD.
2. Progressive Supranuclear Palsy (PSP)
PSP is characterized by problems with eye movements and balance.
Symptoms: Frequent falls (often backwards), difficulty looking up or down, and personality changes.
Distinction: Tremor is less common in PSP than in PD.
3. Corticobasal Degeneration (CBD)
This is a rare form that affects one side of the body more than the other.
Symptoms: "Alien limb phenomenon" (where a limb seems to move on its own), severe stiffness, and difficulty with complex movements (apraxia).
4. Lewy Body Dementia (LBD)
While PD can lead to dementia later in life, LBD presents with cognitive decline and hallucinations early in the disease course, often before or at the same time as movement issues.
5. Vascular Parkinsonism
Caused by multiple small strokes in the brain area controlling movement.
Symptoms: Often affects the legs more than the upper body ("lower body Parkinsonism"), leading to a shuffling gait.
Response to Meds: Poor response to Levodopa.
Advanced imaging, such as MRI scans, can help doctors differentiate between typical Parkinson's and its variants by looking for specific patterns of atrophy:
Why Distinction Matters
Diagnosing the correct variant is vital because:
Medication Management: Atypical forms often do not respond well to standard Parkinson's drugs like Levodopa.
Prognosis: Variants often progress faster and require different support strategies.
Symptom Management: Treatments need to target specific issues like low blood pressure in MSA or swallowing difficulties in PSP.
A thorough clinical examination by a specialist is the primary method for distinguishing between these complex disorders:

Key Takeaways
Not all tremors are Parkinson's: A thorough neurological exam is needed to rule out variants.
Watch for "Red Flags": Early falls, hallucinations, or severe blood pressure drops suggest a variant.
Medication response is a clue: If Levodopa doesn't help, it might be Atypical Parkinsonism.
Therapy is key: Regardless of the type, physical and speech therapy are essential to maintain function.
FAQ
Q: Can a blood test diagnose these variants?
A: No, there is currently no definitive blood test. Diagnosis is based on clinical history, physical exams, and sometimes MRI scans to look for specific brain atrophy patterns.
Q: Is Atypical Parkinsonism hereditary?
A: Most cases are sporadic, meaning they happen randomly. However, genetics can play a role in some rare forms.
Q: Can you have both Parkinson's and a variant?
A: It is rare to have both. Usually, it is one specific underlying pathology causing the symptoms.

