Cognitive Changes in Parkinson’s Disease: Symptoms, Causes & Management
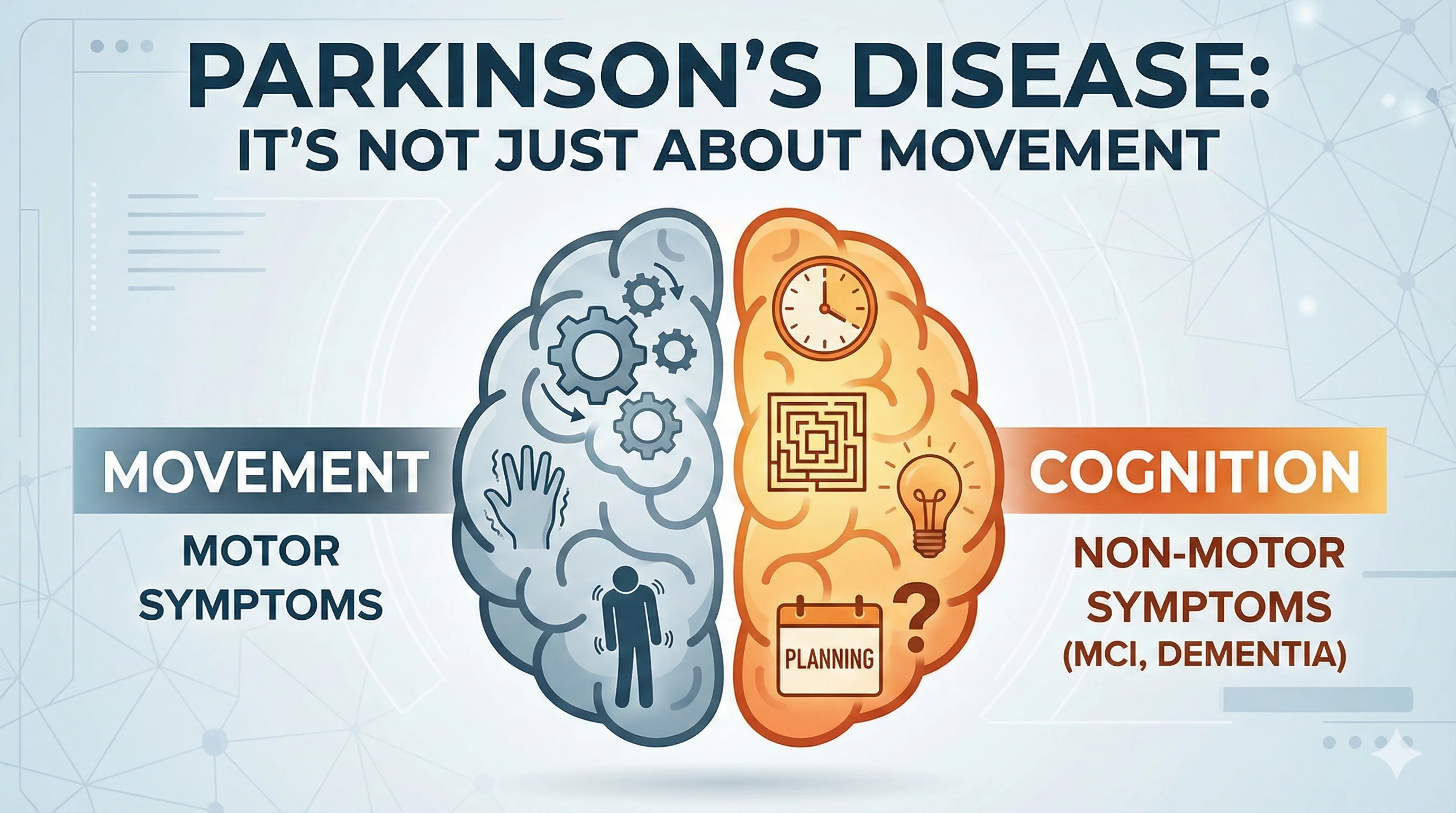
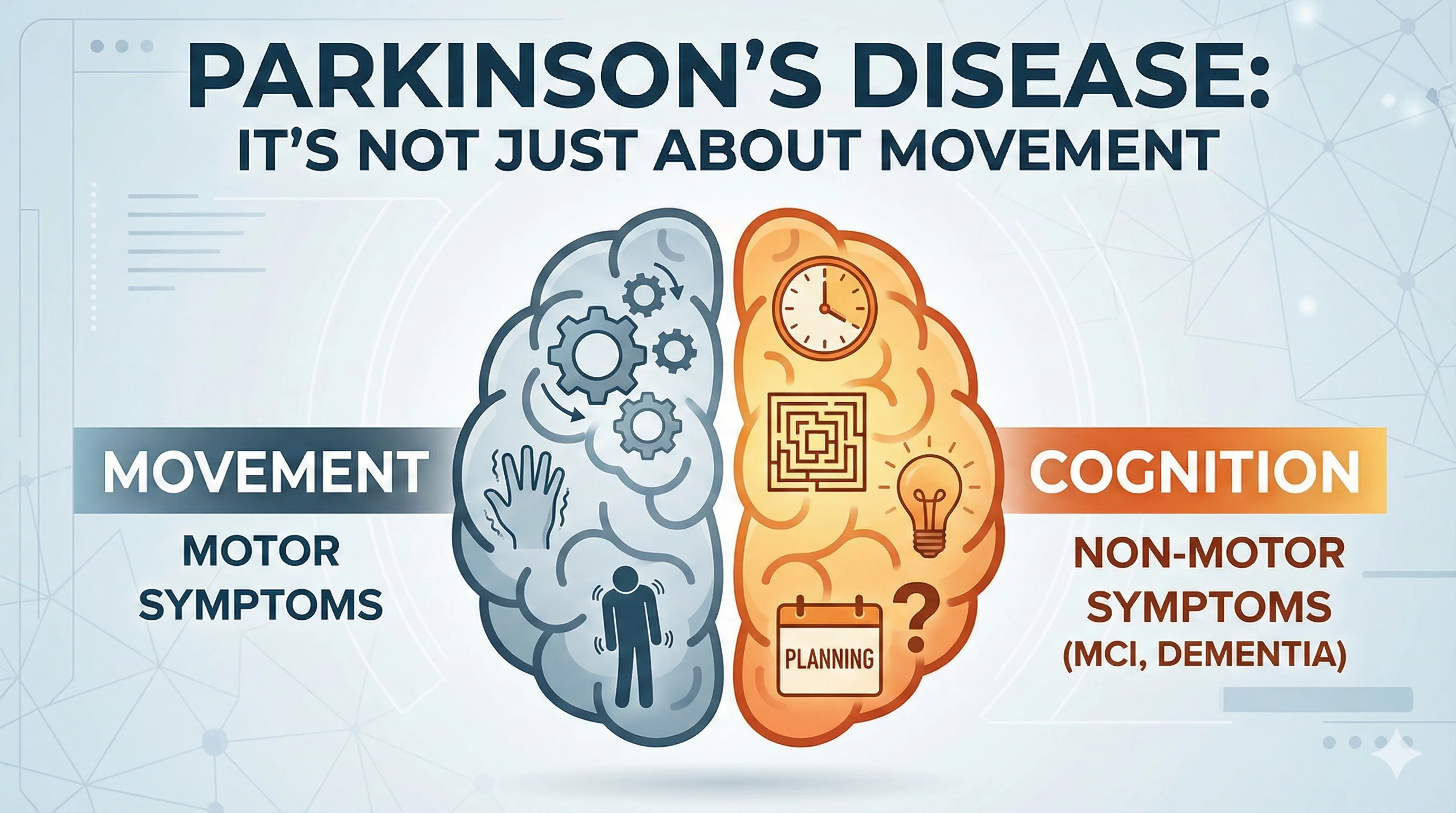
While Parkinson’s Disease (PD) is primarily a movement disorder, cognitive changes are a common non-motor symptom. These can range from mild difficulties with multitasking and planning (Mild Cognitive Impairment) to more severe deficits that impact daily life (Parkinson’s Disease Dementia). These changes are caused by a drop in dopamine and other neurotransmitters in the brain areas responsible for thinking and memory.
It's Not Just About Movement
The same brain chemical changes that cause tremors and stiffness can also affect how the brain processes information. Cognitive issues in PD are distinct from Alzheimer's disease. While Alzheimer's primarily affects memory storage (forgetting names or events), Parkinson's primarily affects executive function (how we organize, plan, and process information).
Common Cognitive Symptoms
1. Executive Dysfunction
Planning: Trouble organizing a complex task (like cooking a meal with multiple steps).
Multitasking: Difficulty doing two things at once (e.g., walking and talking).
Problem Solving: Struggling to figure out solutions to new problems.
2. Attention and Speed
Bradyphrenia: Slowness of thought. It takes longer to process information or respond to a question.
Focus: Difficulty maintaining attention or getting easily distracted.
3. Visuospatial Skills
Depth Perception: Trouble judging distances, which can increase the risk of falls.
Navigation: Getting lost in familiar places.
4. Memory
Retrieval: In PD, the memory is usually there, but it takes longer to find it. A hint often helps (unlike in Alzheimer's).
Mild Cognitive Impairment (MCI) vs. Dementia
PD-MCI: The person has cognitive problems that are noticeable but do not prevent them from living independently. About 20-50% of patients have MCI at diagnosis.
PD Dementia (PDD): Cognitive decline becomes severe enough to interfere with daily life and independence. This typically occurs in the advanced stages of the disease (usually 10+ years after diagnosis).
Management and Support
1. Medication Review
Reduce Anticholinergics: Some drugs used for bladder or tremor can worsen memory.
Cholinesterase Inhibitors: Drugs like Rivastigmine or Donepezil (used in Alzheimer's) can also help with cognitive symptoms in PD.
2. Cognitive Stimulation
"Use it or lose it": Puzzles, reading, learning a new language, or social engagement help build "cognitive reserve."
Exercise: Physical exercise is the #1 way to protect the brain and improve blood flow.
3. Practical Strategies
One thing at a time: Avoid multitasking. Focus on one task until it is done.
Routine: Keep a strict daily schedule.
Visual Cues: Use calendars, sticky notes, and alarms.
Patience: Caregivers should give the person extra time to answer questions.
Key Takeaways
Slowness is not stupidity: The person understands; they just need more time to process.
Hallucinations are a red flag: If cognitive decline is accompanied by seeing things that aren't there, see a doctor immediately.
Depression mimics dementia: Treating depression can often improve cognitive function ("Pseudodementia").
Early screening: Regular cognitive assessments help track changes.
FAQ
Q: Will everyone with Parkinson's get dementia?
A: No, not everyone. While the risk increases with age and disease duration, many people maintain good cognitive function for decades.
Q: How is this different from Alzheimer's?
A: Alzheimer's starts with memory loss. Parkinson's cognitive issues start with attention, planning, and speed of processing.
Q: Can diet help?
A: A Mediterranean diet (rich in healthy fats, fish, and veggies) is linked to better brain health.
While Parkinson’s Disease (PD) is primarily a movement disorder, cognitive changes are a common non-motor symptom. These can range from mild difficulties with multitasking and planning (Mild Cognitive Impairment) to more severe deficits that impact daily life (Parkinson’s Disease Dementia). These changes are caused by a drop in dopamine and other neurotransmitters in the brain areas responsible for thinking and memory.
It's Not Just About Movement
The same brain chemical changes that cause tremors and stiffness can also affect how the brain processes information. Cognitive issues in PD are distinct from Alzheimer's disease. While Alzheimer's primarily affects memory storage (forgetting names or events), Parkinson's primarily affects executive function (how we organize, plan, and process information).
Common Cognitive Symptoms
1. Executive Dysfunction
Planning: Trouble organizing a complex task (like cooking a meal with multiple steps).
Multitasking: Difficulty doing two things at once (e.g., walking and talking).
Problem Solving: Struggling to figure out solutions to new problems.
2. Attention and Speed
Bradyphrenia: Slowness of thought. It takes longer to process information or respond to a question.
Focus: Difficulty maintaining attention or getting easily distracted.
3. Visuospatial Skills
Depth Perception: Trouble judging distances, which can increase the risk of falls.
Navigation: Getting lost in familiar places.
4. Memory
Retrieval: In PD, the memory is usually there, but it takes longer to find it. A hint often helps (unlike in Alzheimer's).
Mild Cognitive Impairment (MCI) vs. Dementia
PD-MCI: The person has cognitive problems that are noticeable but do not prevent them from living independently. About 20-50% of patients have MCI at diagnosis.
PD Dementia (PDD): Cognitive decline becomes severe enough to interfere with daily life and independence. This typically occurs in the advanced stages of the disease (usually 10+ years after diagnosis).
Management and Support
1. Medication Review
Reduce Anticholinergics: Some drugs used for bladder or tremor can worsen memory.
Cholinesterase Inhibitors: Drugs like Rivastigmine or Donepezil (used in Alzheimer's) can also help with cognitive symptoms in PD.
2. Cognitive Stimulation
"Use it or lose it": Puzzles, reading, learning a new language, or social engagement help build "cognitive reserve."
Exercise: Physical exercise is the #1 way to protect the brain and improve blood flow.
3. Practical Strategies
One thing at a time: Avoid multitasking. Focus on one task until it is done.
Routine: Keep a strict daily schedule.
Visual Cues: Use calendars, sticky notes, and alarms.
Patience: Caregivers should give the person extra time to answer questions.
Key Takeaways
Slowness is not stupidity: The person understands; they just need more time to process.
Hallucinations are a red flag: If cognitive decline is accompanied by seeing things that aren't there, see a doctor immediately.
Depression mimics dementia: Treating depression can often improve cognitive function ("Pseudodementia").
Early screening: Regular cognitive assessments help track changes.
FAQ
Q: Will everyone with Parkinson's get dementia?
A: No, not everyone. While the risk increases with age and disease duration, many people maintain good cognitive function for decades.
Q: How is this different from Alzheimer's?
A: Alzheimer's starts with memory loss. Parkinson's cognitive issues start with attention, planning, and speed of processing.
Q: Can diet help?
A: A Mediterranean diet (rich in healthy fats, fish, and veggies) is linked to better brain health.
While Parkinson’s Disease (PD) is primarily a movement disorder, cognitive changes are a common non-motor symptom. These can range from mild difficulties with multitasking and planning (Mild Cognitive Impairment) to more severe deficits that impact daily life (Parkinson’s Disease Dementia). These changes are caused by a drop in dopamine and other neurotransmitters in the brain areas responsible for thinking and memory.
It's Not Just About Movement
The same brain chemical changes that cause tremors and stiffness can also affect how the brain processes information. Cognitive issues in PD are distinct from Alzheimer's disease. While Alzheimer's primarily affects memory storage (forgetting names or events), Parkinson's primarily affects executive function (how we organize, plan, and process information).
Common Cognitive Symptoms
1. Executive Dysfunction
Planning: Trouble organizing a complex task (like cooking a meal with multiple steps).
Multitasking: Difficulty doing two things at once (e.g., walking and talking).
Problem Solving: Struggling to figure out solutions to new problems.
2. Attention and Speed
Bradyphrenia: Slowness of thought. It takes longer to process information or respond to a question.
Focus: Difficulty maintaining attention or getting easily distracted.
3. Visuospatial Skills
Depth Perception: Trouble judging distances, which can increase the risk of falls.
Navigation: Getting lost in familiar places.
4. Memory
Retrieval: In PD, the memory is usually there, but it takes longer to find it. A hint often helps (unlike in Alzheimer's).
Mild Cognitive Impairment (MCI) vs. Dementia
PD-MCI: The person has cognitive problems that are noticeable but do not prevent them from living independently. About 20-50% of patients have MCI at diagnosis.
PD Dementia (PDD): Cognitive decline becomes severe enough to interfere with daily life and independence. This typically occurs in the advanced stages of the disease (usually 10+ years after diagnosis).
Management and Support
1. Medication Review
Reduce Anticholinergics: Some drugs used for bladder or tremor can worsen memory.
Cholinesterase Inhibitors: Drugs like Rivastigmine or Donepezil (used in Alzheimer's) can also help with cognitive symptoms in PD.
2. Cognitive Stimulation
"Use it or lose it": Puzzles, reading, learning a new language, or social engagement help build "cognitive reserve."
Exercise: Physical exercise is the #1 way to protect the brain and improve blood flow.
3. Practical Strategies
One thing at a time: Avoid multitasking. Focus on one task until it is done.
Routine: Keep a strict daily schedule.
Visual Cues: Use calendars, sticky notes, and alarms.
Patience: Caregivers should give the person extra time to answer questions.
Key Takeaways
Slowness is not stupidity: The person understands; they just need more time to process.
Hallucinations are a red flag: If cognitive decline is accompanied by seeing things that aren't there, see a doctor immediately.
Depression mimics dementia: Treating depression can often improve cognitive function ("Pseudodementia").
Early screening: Regular cognitive assessments help track changes.
FAQ
Q: Will everyone with Parkinson's get dementia?
A: No, not everyone. While the risk increases with age and disease duration, many people maintain good cognitive function for decades.
Q: How is this different from Alzheimer's?
A: Alzheimer's starts with memory loss. Parkinson's cognitive issues start with attention, planning, and speed of processing.
Q: Can diet help?
A: A Mediterranean diet (rich in healthy fats, fish, and veggies) is linked to better brain health.

