Parkinson’s Disease Psychosis: Hallucinations, Delusions & Treatment


Hallucinations (seeing things that aren't there) and delusions (believing things that aren't true) are distressing symptoms that can occur in Parkinson’s Disease (PD), usually in later stages. This condition, known as Parkinson’s Disease Psychosis, is often caused by a combination of the disease progression itself and the side effects of dopamine medications. It is a major cause of caregiver stress but can be treated with medication adjustments and specialized antipsychotics.
Seeing the Unseen
For a patient, seeing a stranger in the living room or a cat on the bed when no one is there can be terrifying. For the caregiver, being accused of stealing or infidelity (delusions) is heartbreaking. These symptoms are part of the neuropsychiatric spectrum of Parkinson's.
Types of Hallucinations
1. Visual Hallucinations (Most Common)
Passage Hallucinations: Seeing a shadow or person dart across the periphery of vision.
Presence Hallucinations: The strong feeling that someone is standing behind you or in the room.
Formed Hallucinations: Seeing fully formed people, animals, or objects. These are often non-threatening initially (e.g., seeing small children or pets).
2. Auditory Hallucinations
Hearing voices or music. This is less common in PD than visual hallucinations.
3. Delusions
False, fixed beliefs that are not based in reality.
Paranoia: Believing the spouse is cheating or the caregiver is poisoning the food.
Theft: Believing money or items are being stolen.
Causes
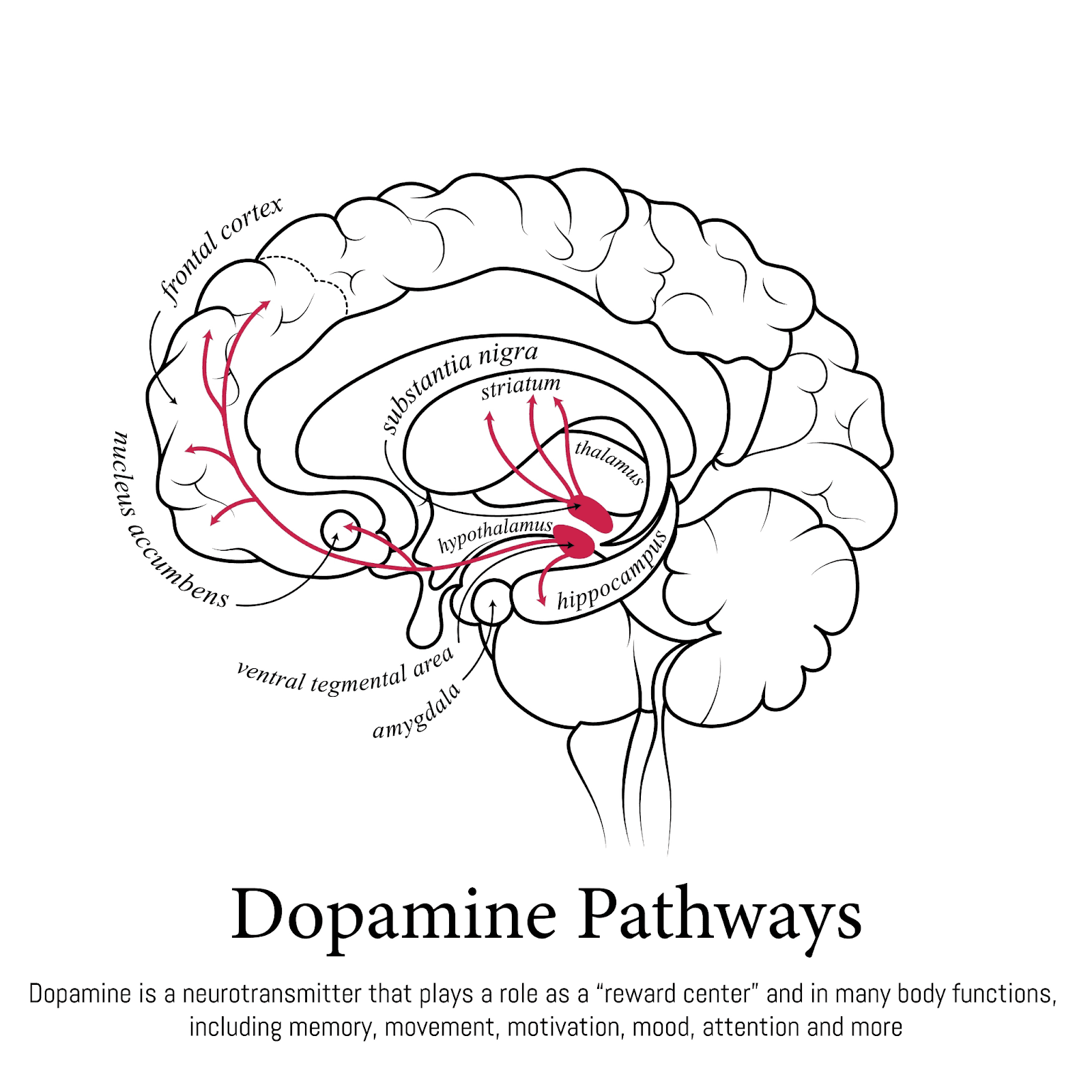
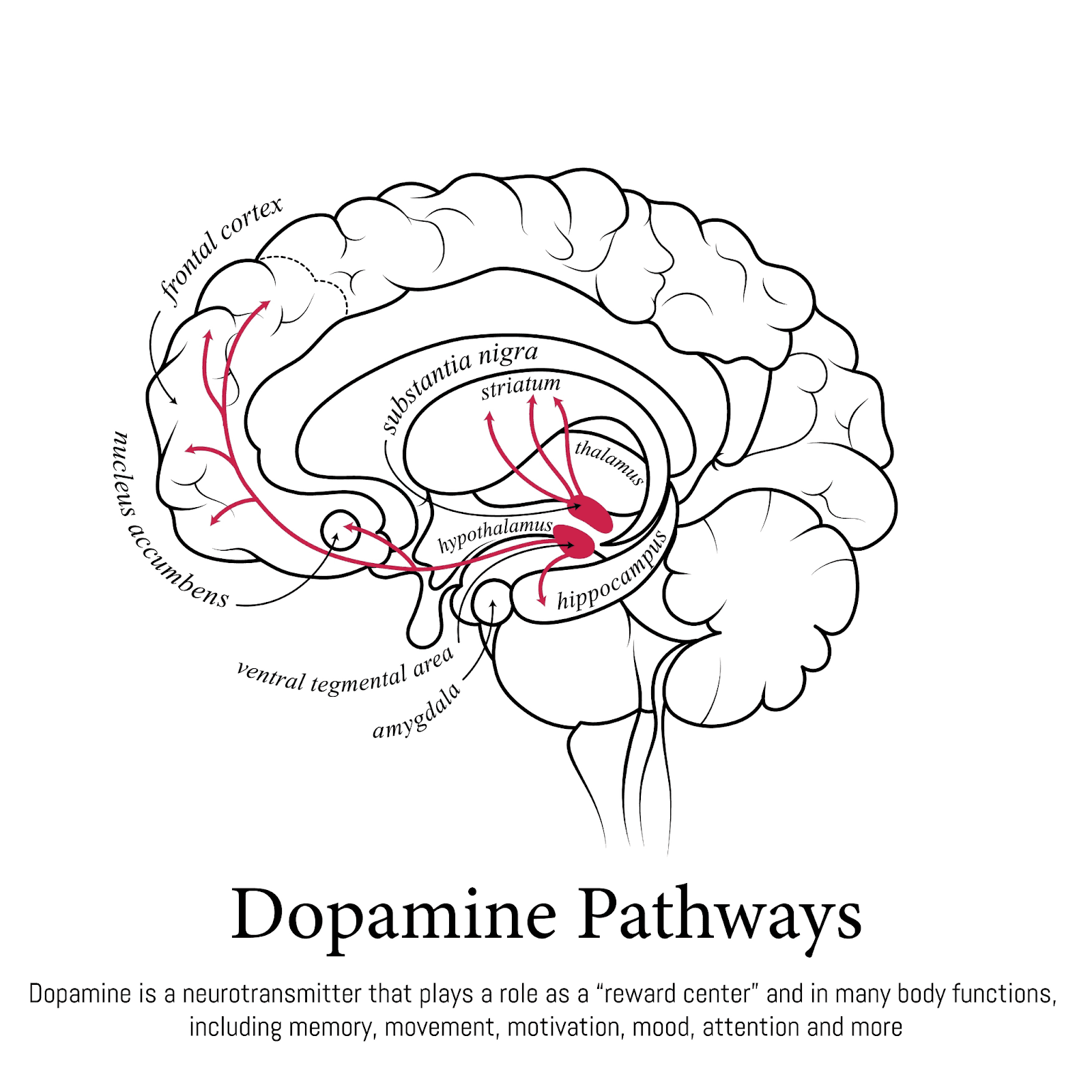
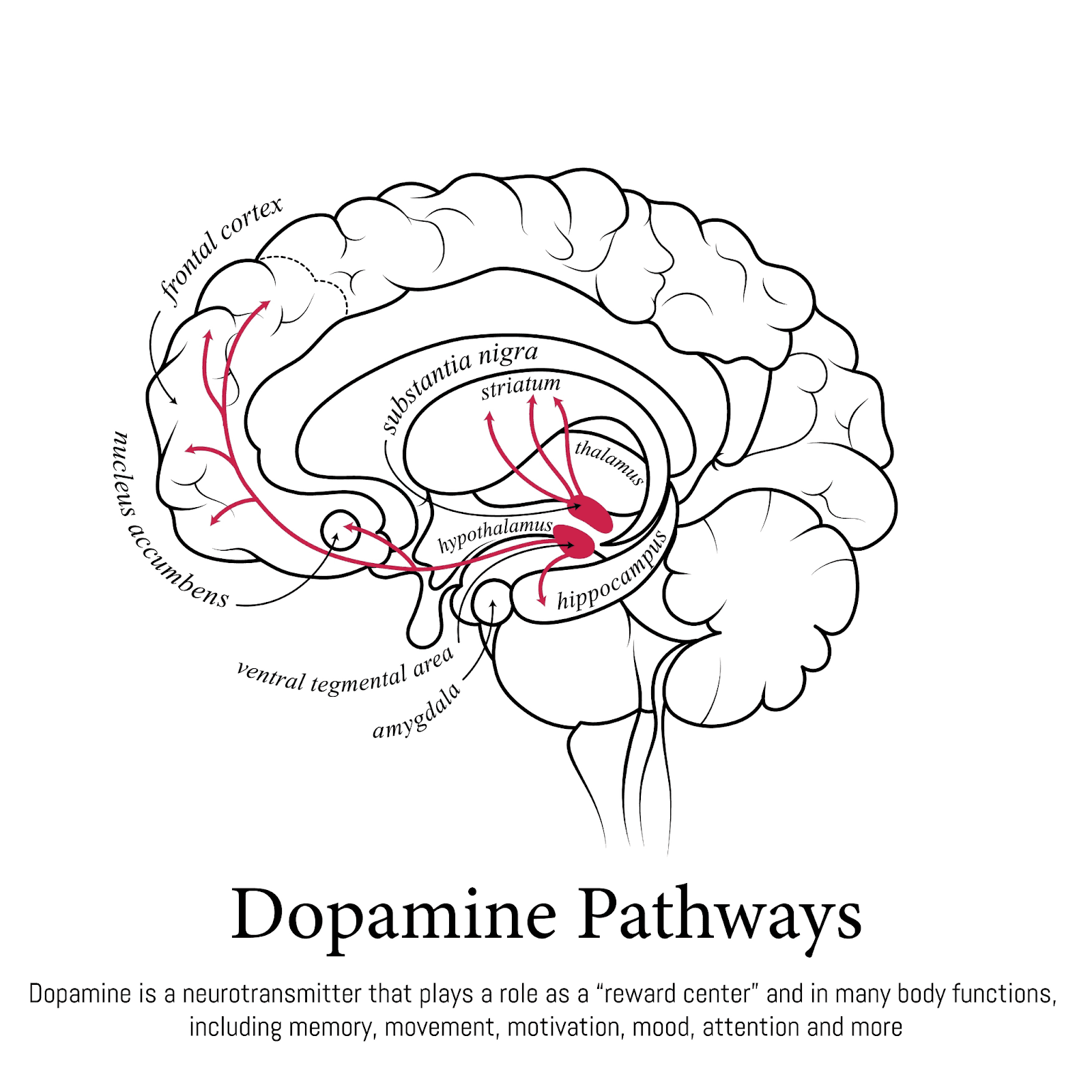
Medication Side Effects: Dopamine replacement therapy (Levodopa, Dopamine Agonists) increases dopamine in the brain. While this helps movement, too much dopamine in the cognitive centers can cause psychosis.
Disease Progression: Lewy body spread to the temporal and parietal lobes of the brain.
Triggers: Infections (UTI, pneumonia), dehydration, or sleep deprivation can trigger sudden hallucinations (delirium).
Management Strategies
1. Rule Out Medical Causes
Before changing PD meds, the doctor will check for infections (UTI is a common culprit) or metabolic imbalances.
2. Medication Adjustment
The neurologist may reduce Parkinson's medications in a specific order to stop hallucinations without worsening motor symptoms:
Stop Anticholinergics.
Stop Amantadine.
Stop Dopamine Agonists.
Reduce Levodopa (last resort).
3. Antipsychotic Medication
If reducing PD meds makes movement too difficult, the doctor may add an antipsychotic.
Clozapine & Quetiapine: Traditional choices that don't worsen motor symptoms too much.
Pimavanserin (Nuplazid): A newer drug specifically approved for PD psychosis. It works on serotonin receptors, not dopamine, so it doesn't worsen motor symptoms at all.
4. Caregiver Tips
Don't argue: You cannot argue someone out of a delusion. It is real to them.
Reassure: "I know you see the cat, but I don't. You are safe."
Lighting: Keep rooms well-lit in the evening to reduce shadows.
Key Takeaways
Insight matters: In early stages, patients often know the hallucination isn't real ("I see a dog, but I know we don't have a dog"). Losing this insight marks a progression.
Report early: Don't wait until the visions are scary. Tell the doctor about even "minor" shadows.
Check for UTI: Sudden confusion + hallucinations = Check urine first.
Safety: Delusions can lead to wandering or aggression.
FAQ
Q: Are hallucinations a sign of insanity?
A: No, they are a chemical imbalance in the brain, just like the tremor is a chemical imbalance.
Q: Will they go away?
A: With treatment (medication adjustment), they can often be reduced or eliminated.
Q: Can I use regular antipsychotics like Haldol?
A: NO. Typical antipsychotics (like Haloperidol) block dopamine and can cause severe, permanent worsening of Parkinson's symptoms (Neuroleptic Malignant Syndrome). Always see a specialist.
Hallucinations (seeing things that aren't there) and delusions (believing things that aren't true) are distressing symptoms that can occur in Parkinson’s Disease (PD), usually in later stages. This condition, known as Parkinson’s Disease Psychosis, is often caused by a combination of the disease progression itself and the side effects of dopamine medications. It is a major cause of caregiver stress but can be treated with medication adjustments and specialized antipsychotics.
Seeing the Unseen
For a patient, seeing a stranger in the living room or a cat on the bed when no one is there can be terrifying. For the caregiver, being accused of stealing or infidelity (delusions) is heartbreaking. These symptoms are part of the neuropsychiatric spectrum of Parkinson's.
Types of Hallucinations
1. Visual Hallucinations (Most Common)
Passage Hallucinations: Seeing a shadow or person dart across the periphery of vision.
Presence Hallucinations: The strong feeling that someone is standing behind you or in the room.
Formed Hallucinations: Seeing fully formed people, animals, or objects. These are often non-threatening initially (e.g., seeing small children or pets).
2. Auditory Hallucinations
Hearing voices or music. This is less common in PD than visual hallucinations.
3. Delusions
False, fixed beliefs that are not based in reality.
Paranoia: Believing the spouse is cheating or the caregiver is poisoning the food.
Theft: Believing money or items are being stolen.
Causes
Medication Side Effects: Dopamine replacement therapy (Levodopa, Dopamine Agonists) increases dopamine in the brain. While this helps movement, too much dopamine in the cognitive centers can cause psychosis.
Disease Progression: Lewy body spread to the temporal and parietal lobes of the brain.
Triggers: Infections (UTI, pneumonia), dehydration, or sleep deprivation can trigger sudden hallucinations (delirium).
Management Strategies
1. Rule Out Medical Causes
Before changing PD meds, the doctor will check for infections (UTI is a common culprit) or metabolic imbalances.
2. Medication Adjustment
The neurologist may reduce Parkinson's medications in a specific order to stop hallucinations without worsening motor symptoms:
Stop Anticholinergics.
Stop Amantadine.
Stop Dopamine Agonists.
Reduce Levodopa (last resort).
3. Antipsychotic Medication
If reducing PD meds makes movement too difficult, the doctor may add an antipsychotic.
Clozapine & Quetiapine: Traditional choices that don't worsen motor symptoms too much.
Pimavanserin (Nuplazid): A newer drug specifically approved for PD psychosis. It works on serotonin receptors, not dopamine, so it doesn't worsen motor symptoms at all.
4. Caregiver Tips
Don't argue: You cannot argue someone out of a delusion. It is real to them.
Reassure: "I know you see the cat, but I don't. You are safe."
Lighting: Keep rooms well-lit in the evening to reduce shadows.
Key Takeaways
Insight matters: In early stages, patients often know the hallucination isn't real ("I see a dog, but I know we don't have a dog"). Losing this insight marks a progression.
Report early: Don't wait until the visions are scary. Tell the doctor about even "minor" shadows.
Check for UTI: Sudden confusion + hallucinations = Check urine first.
Safety: Delusions can lead to wandering or aggression.
FAQ
Q: Are hallucinations a sign of insanity?
A: No, they are a chemical imbalance in the brain, just like the tremor is a chemical imbalance.
Q: Will they go away?
A: With treatment (medication adjustment), they can often be reduced or eliminated.
Q: Can I use regular antipsychotics like Haldol?
A: NO. Typical antipsychotics (like Haloperidol) block dopamine and can cause severe, permanent worsening of Parkinson's symptoms (Neuroleptic Malignant Syndrome). Always see a specialist.
Hallucinations (seeing things that aren't there) and delusions (believing things that aren't true) are distressing symptoms that can occur in Parkinson’s Disease (PD), usually in later stages. This condition, known as Parkinson’s Disease Psychosis, is often caused by a combination of the disease progression itself and the side effects of dopamine medications. It is a major cause of caregiver stress but can be treated with medication adjustments and specialized antipsychotics.
Seeing the Unseen
For a patient, seeing a stranger in the living room or a cat on the bed when no one is there can be terrifying. For the caregiver, being accused of stealing or infidelity (delusions) is heartbreaking. These symptoms are part of the neuropsychiatric spectrum of Parkinson's.
Types of Hallucinations
1. Visual Hallucinations (Most Common)
Passage Hallucinations: Seeing a shadow or person dart across the periphery of vision.
Presence Hallucinations: The strong feeling that someone is standing behind you or in the room.
Formed Hallucinations: Seeing fully formed people, animals, or objects. These are often non-threatening initially (e.g., seeing small children or pets).
2. Auditory Hallucinations
Hearing voices or music. This is less common in PD than visual hallucinations.
3. Delusions
False, fixed beliefs that are not based in reality.
Paranoia: Believing the spouse is cheating or the caregiver is poisoning the food.
Theft: Believing money or items are being stolen.
Causes
Medication Side Effects: Dopamine replacement therapy (Levodopa, Dopamine Agonists) increases dopamine in the brain. While this helps movement, too much dopamine in the cognitive centers can cause psychosis.
Disease Progression: Lewy body spread to the temporal and parietal lobes of the brain.
Triggers: Infections (UTI, pneumonia), dehydration, or sleep deprivation can trigger sudden hallucinations (delirium).
Management Strategies
1. Rule Out Medical Causes
Before changing PD meds, the doctor will check for infections (UTI is a common culprit) or metabolic imbalances.
2. Medication Adjustment
The neurologist may reduce Parkinson's medications in a specific order to stop hallucinations without worsening motor symptoms:
Stop Anticholinergics.
Stop Amantadine.
Stop Dopamine Agonists.
Reduce Levodopa (last resort).
3. Antipsychotic Medication
If reducing PD meds makes movement too difficult, the doctor may add an antipsychotic.
Clozapine & Quetiapine: Traditional choices that don't worsen motor symptoms too much.
Pimavanserin (Nuplazid): A newer drug specifically approved for PD psychosis. It works on serotonin receptors, not dopamine, so it doesn't worsen motor symptoms at all.
4. Caregiver Tips
Don't argue: You cannot argue someone out of a delusion. It is real to them.
Reassure: "I know you see the cat, but I don't. You are safe."
Lighting: Keep rooms well-lit in the evening to reduce shadows.
Key Takeaways
Insight matters: In early stages, patients often know the hallucination isn't real ("I see a dog, but I know we don't have a dog"). Losing this insight marks a progression.
Report early: Don't wait until the visions are scary. Tell the doctor about even "minor" shadows.
Check for UTI: Sudden confusion + hallucinations = Check urine first.
Safety: Delusions can lead to wandering or aggression.
FAQ
Q: Are hallucinations a sign of insanity?
A: No, they are a chemical imbalance in the brain, just like the tremor is a chemical imbalance.
Q: Will they go away?
A: With treatment (medication adjustment), they can often be reduced or eliminated.
Q: Can I use regular antipsychotics like Haldol?
A: NO. Typical antipsychotics (like Haloperidol) block dopamine and can cause severe, permanent worsening of Parkinson's symptoms (Neuroleptic Malignant Syndrome). Always see a specialist.

